Corneal Collagen Cross-Linking
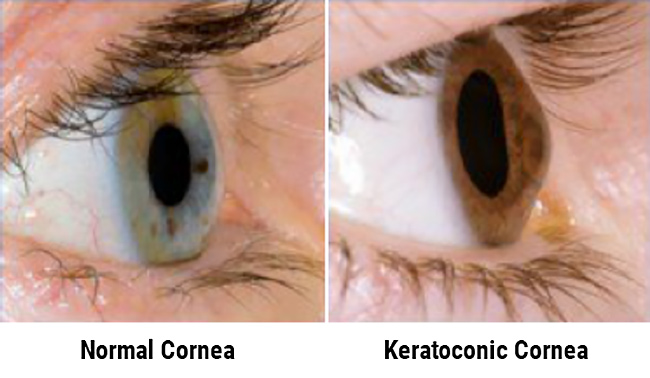
A New Keratoconus Treatment, Stops Keratoconus from Progressing
As a leading cornea specialist in the Washington, DC area, Dr. Daniel Sarezky is one of the few eye surgeons to offer Corneal Cross-Linking to patients affected by keratoconus and corneal ectasia. Dr. Sarezky performs this innovative procedure more than any another provider in the state of Maryland.