Glaucoma Eye Drops
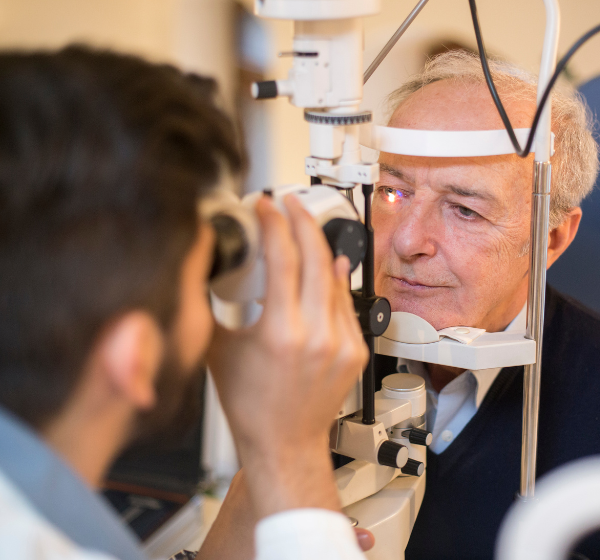
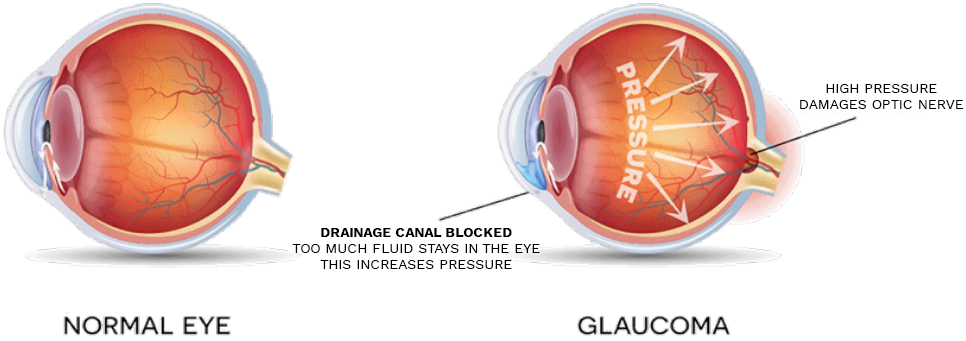
With Visionary Eye Doctors, you have many options for glaucoma treatment in the Washington, DC, DC area. Prescription Eye Drops for glaucoma help maintain the pressure in your eye at a healthy level and are an important part of the treatment routine for many people. It is important to notify your doctor of any other medications you may be taking (including over-the-counter items like vitamins, aspirin, and herbal supplements) and about any allergies you may have.
Treatment requires monitoring eye pressure and measuring changes in the peripheral visual field. Controlling glaucoma usually means maintaining eye pressure at an acceptable level when there has been little or no loss of the visual field.
We are one of the few centers in the Washington, DC, DC metro area to offer our Glaucoma patients the Icare.
The Icare home tonometer is one of the first methods for 24HR monitoring outside normal clinic hours which may help identify IOP variations and spikes.
Self-tonometry with the Icare® HOME is designed to gather additional intraocular pressure (IOP) information from the patient. The device records IOP, date, time, eye, and a quality score which is not displayed to the patient. The data is retrieved by a healthcare provider via Icare® LINK software.
Some of the most common procedures we offer to treat glaucoma include selective laser trabeculoplasty (SLT), laser peripheral iridotomy (LPI), trabeculectomy, or shunt placement.


![9947 Website Background match -Dr Medina - 2nd edit[65] Dr. Medina Headshot](https://www.voeyedr.com/wp-content/uploads/2023/11/9947-Website-Background-match-Dr-Medina-2nd-edit65.png)