Signs of Cataracts: What to Look For and When to Seek Help
Quick Take: Cataracts can cause:
-
- Cloudy vision
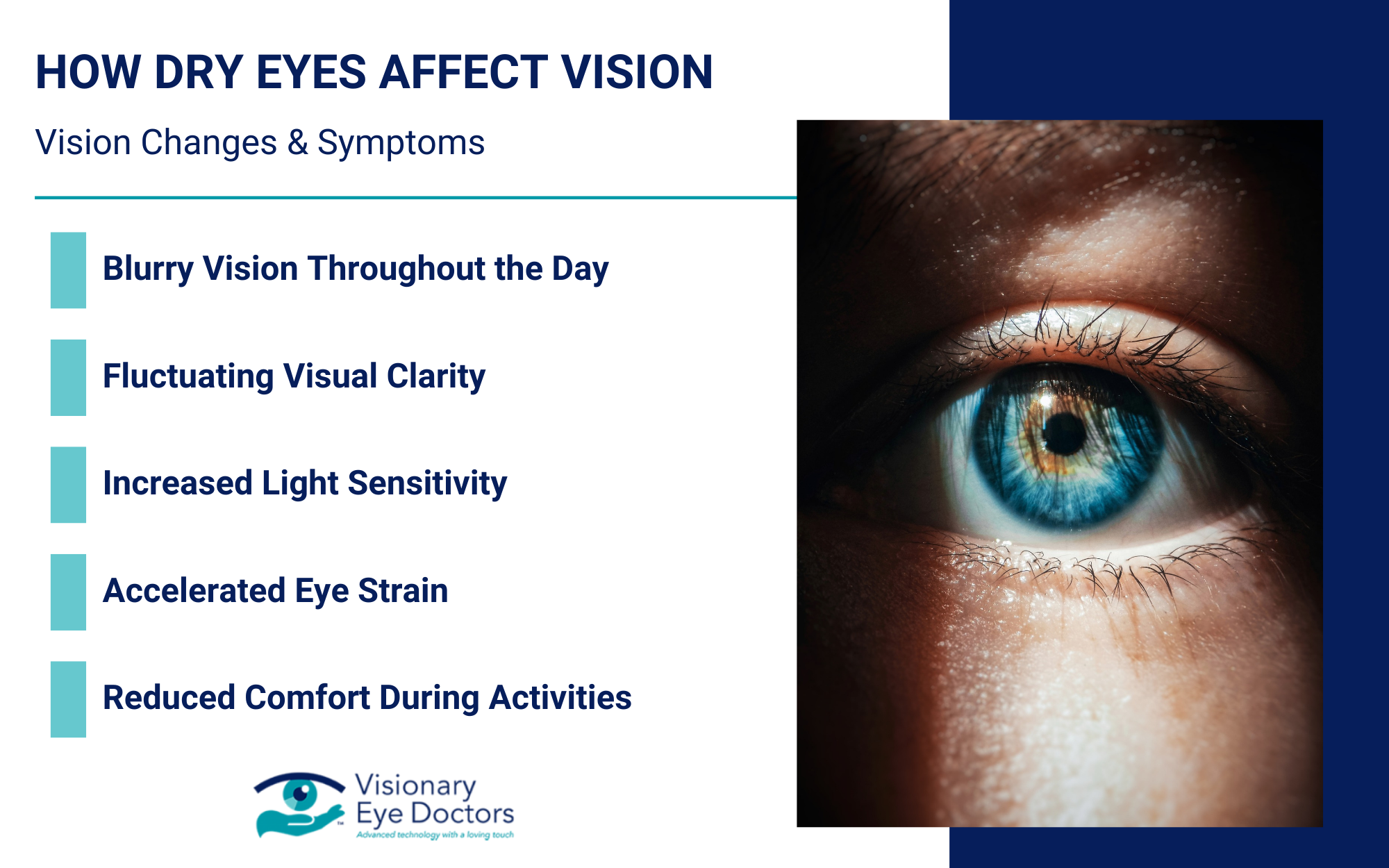
- Increased light sensitivity
- Faded colors
- Problems seeing at night
These cataract symptoms often develop slowly, and recognizing them early can help you seek appropriate treatment before your daily activities are affected.
Cataracts are one of the most common eye conditions, especially among people over 60. They occur when the eye’s natural lens becomes cloudy, similar to looking through a foggy window. While age-related cataracts develop gradually, knowing the early signs helps you maintain clear vision and quality of life.
In this blog, you’ll learn:
- What cataracts are and why they form
- Common signs like cloudy vision and light sensitivity
- When to see an eye doctor
- Treatment options, including cataract surgery
- How to protect your vision over time
What Are Cataracts?
Cataracts form when proteins in the eye’s lens clump together, creating a clouded lens that scatters light and reduces visual clarity. This buildup leads to vision problems like blurry vision, glare, and difficulty reading or driving.
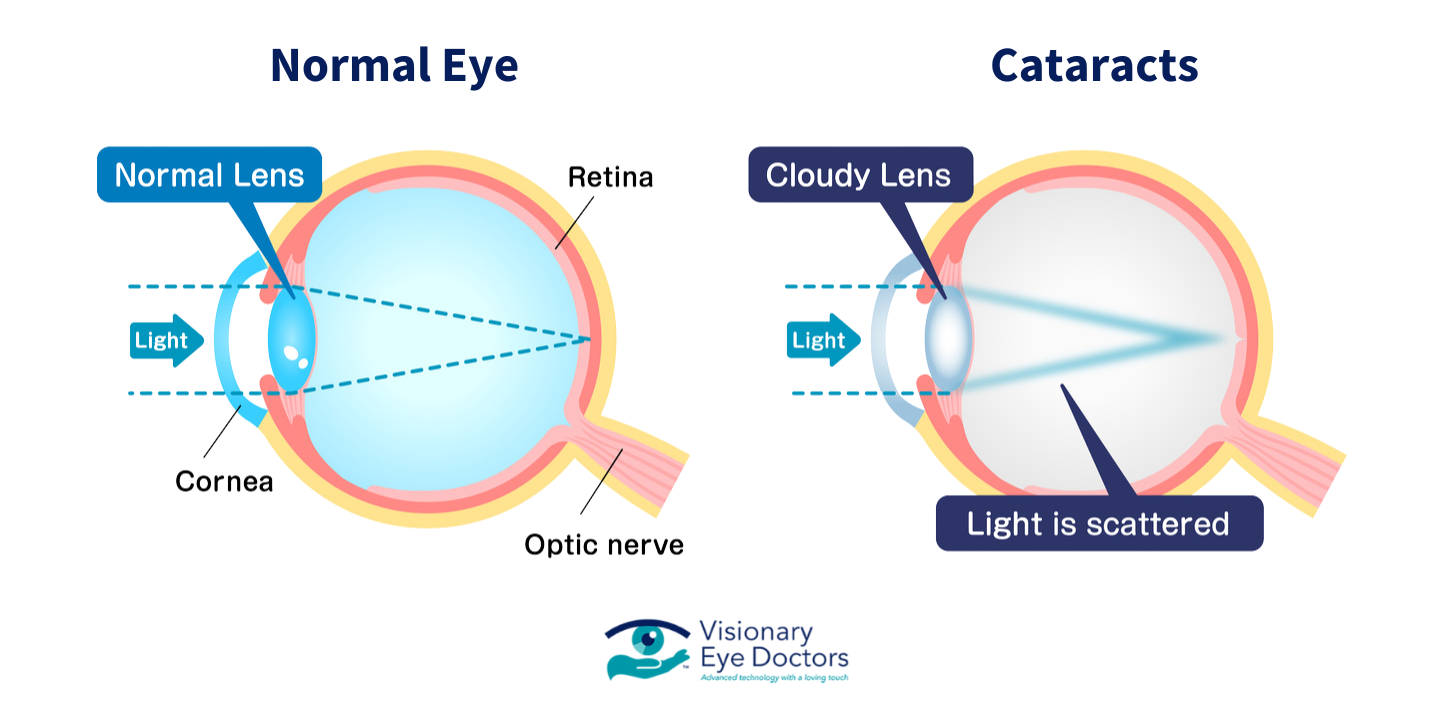
The lens sits behind your iris (the colored part of your eye) and works much like a camera lens, focusing light onto the retina at the back of your eye. A clear lens allows for sharp images on your retina, but when a cataract clouds the lens, your vision becomes blurred, similar to looking through a dirty windshield or a fogged-up window.
Types of Cataracts
There are several types of cataracts, each affecting different parts of the lens:
- Nuclear cataract: Forms in the center of the lens and is most commonly related to aging. These cataracts often temporarily improve near vision before overall vision deteriorates.
- Cortical cataract: Starts at the edges of the lens and gradually moves inward. These appear as wedge-shaped cloudy areas that extend from the outside edge toward the center, often resembling spokes on a wheel.
- Posterior subcapsular cataract: Develops at the back of the lens, often leading to difficulty with bright light and night vision. These tend to progress faster than other types and frequently affect people with diabetes or those taking steroid medications.
- Congenital cataract: Present at birth or during childhood (also known as pediatric cataracts). These can be hereditary or result from an infection during pregnancy.
What Causes Cataracts?
Cataracts can result from a range of factors, including:
- Age, especially after 60
- Medical conditions like diabetes or macular degeneration
- Long-term exposure to bright sunlight or toxic substances
- Smoking or alcohol use
- Long-term steroid use
- Previous eye injuries, retinal detachment, or eye surgery
- Family history of cataracts
While aging is the primary cause, research suggests that oxidative stress plays a significant role in cataract development. This happens when unstable molecules (free radicals) attack and harm the proteins in the eye’s lens. This damage accumulates over a lifetime, which explains why cataracts become more common as we age.
Early Signs of Cataracts
In the early stages, cataracts may not be obvious, but subtle vision changes often appear.
Common early symptoms include:
- Cloudy vision or a sense that things look dim or hazy
- Difficulty seeing at night or in low-light settings
- Sensitivity to bright light and glare from headlights or sunlight
- Seeing halos around light sources
- Double vision in one eye
- Colors appearing faded or yellowish
- Needing more light to read or complete close-up tasks
- Frequent changes to your lens prescription or contact lenses
These symptoms can come on slowly, which is why regular eye exams are essential.
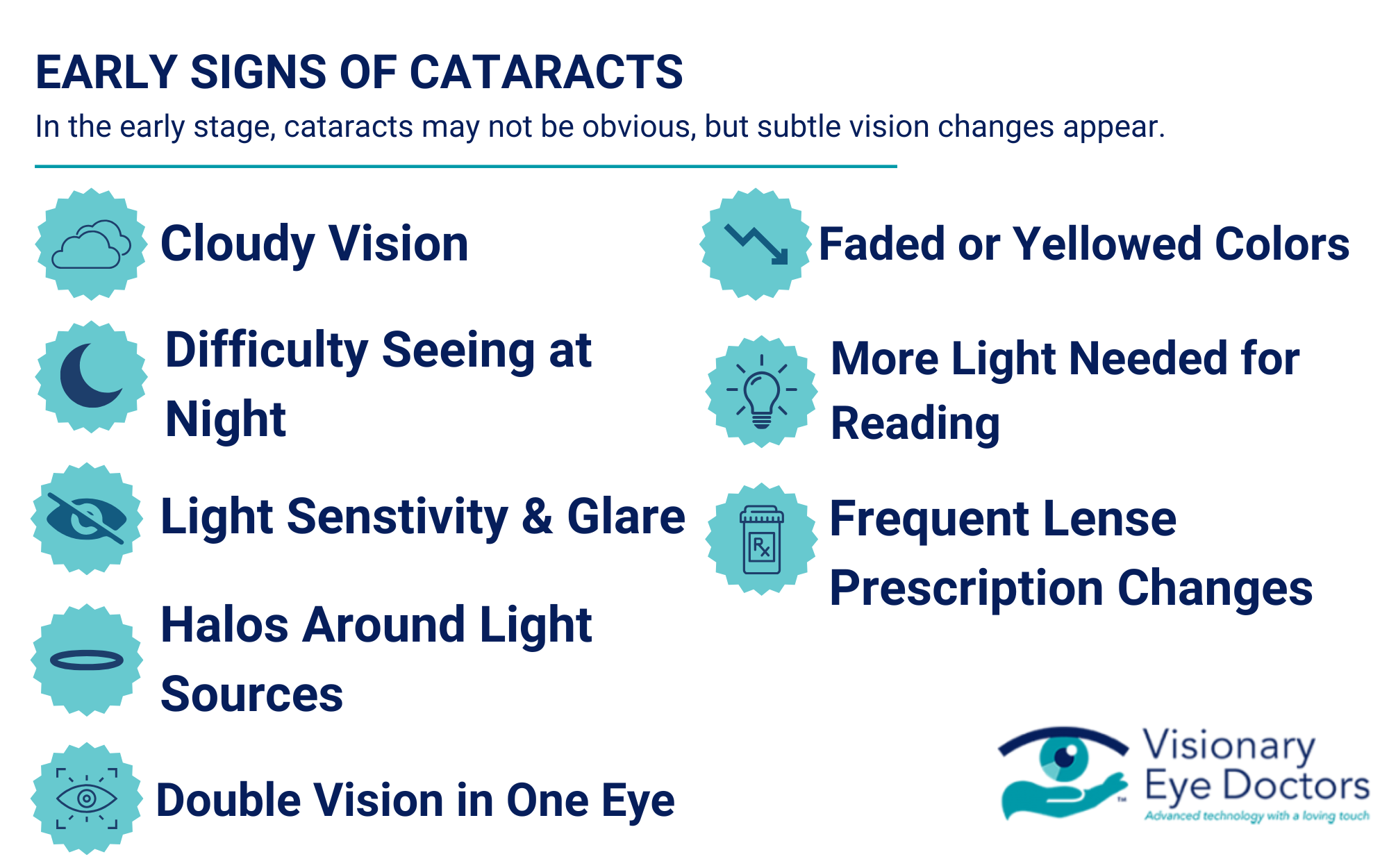
Many people describe early cataract symptoms as similar to looking through a dirty car windshield or a piece of wax paper. You might find yourself cleaning your glasses frequently, thinking they’re dirty, when the problem is actually with your eye’s lens.
When Cataracts Get Worse
As the cataract progresses, the symptoms become more disruptive to your daily activities. You may notice:
- Increasingly blurry or cloudy vision
- Trouble distinguishing colors, especially blues and purples
- Heightened light sensitivity and glare from bright sunlight
- A white or yellow tint in the pupil (a possible sign of a mature cataract)
- Temporary improvement in near vision (“second sight”), followed by worsening overall clarity
These are signs of an advanced cataract, and you should consult an eye doctor promptly.
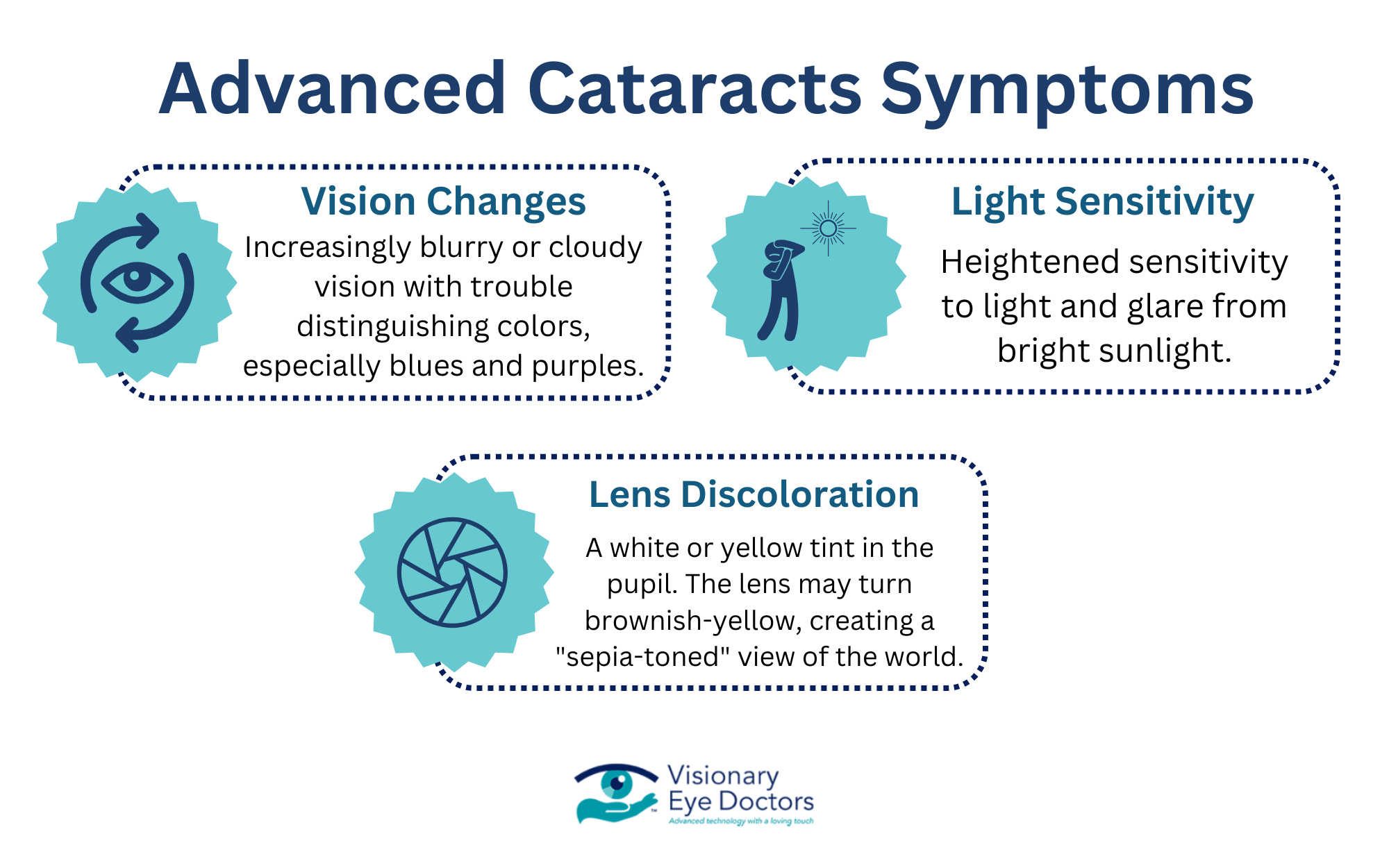
As cataracts mature, the lens may turn a brownish-yellow color, distorting your color perception. Many patients describe this as viewing the world through a sepia-toned filter. This color shift can make it difficult to distinguish between certain hues, particularly in the blue-purple spectrum.
How Cataracts Impact Daily Life
Cataracts can affect your ability to function comfortably at home, work, and on the road.
You might experience:
- Driving difficulties – especially with night vision or glare from headlights
- Reading problems – needing more light or magnification to see small print
- Trouble recognizing faces from a distance
- Difficulty with tasks that require visual detail, like sewing or cooking
If vision loss starts to interfere with normal routines, it’s time to consider your treatment options.
The impact of cataracts often extends beyond just vision problems. Many people experience increased anxiety, particularly around driving at night or in unfamiliar places. Social isolation can occur when individuals begin avoiding activities they once enjoyed because of vision difficulties. Studies show that untreated cataracts significantly increase the risk of falls and accidents, especially in older adults.
When to See an Eye Doctor
You should schedule an eye exam if:
- You notice vision changes that make it harder to perform everyday tasks
- Colors appear dull or yellowed
- You’ve had multiple updates to your glasses or contact lenses
- Glare or halos interfere with driving or reading
- Any of the above symptoms of cataracts are affecting your comfort or independence
Recommended exam schedule:
| Age | Recommended Exam Frequency |
| 40-54 | Every 2-4 years |
| 55-64 | Every 1-3 years |
| 65+ | Every 1-2 years |
| *Patients with underlying conditions (diabetes, family history)* | Annually |
Diagnosing Cataracts
To confirm a cataract diagnosis, your eye doctor may:
- Perform a visual acuity test
- Use a slit-lamp microscope to examine the clouded lens
- Dilate your pupils to inspect the retina
- Test how you respond to glare and how well you perceive contrast
- Evaluate color vision and depth perception
These evaluations help determine the best course of treatment, including whether surgery is needed.
During a comprehensive eye exam, your doctor will also check for other eye conditions that may coexist with cataracts, such as glaucoma or age-related macular degeneration. This thorough approach ensures that all potential vision threats are identified and addressed.
Cataract Treatment Options
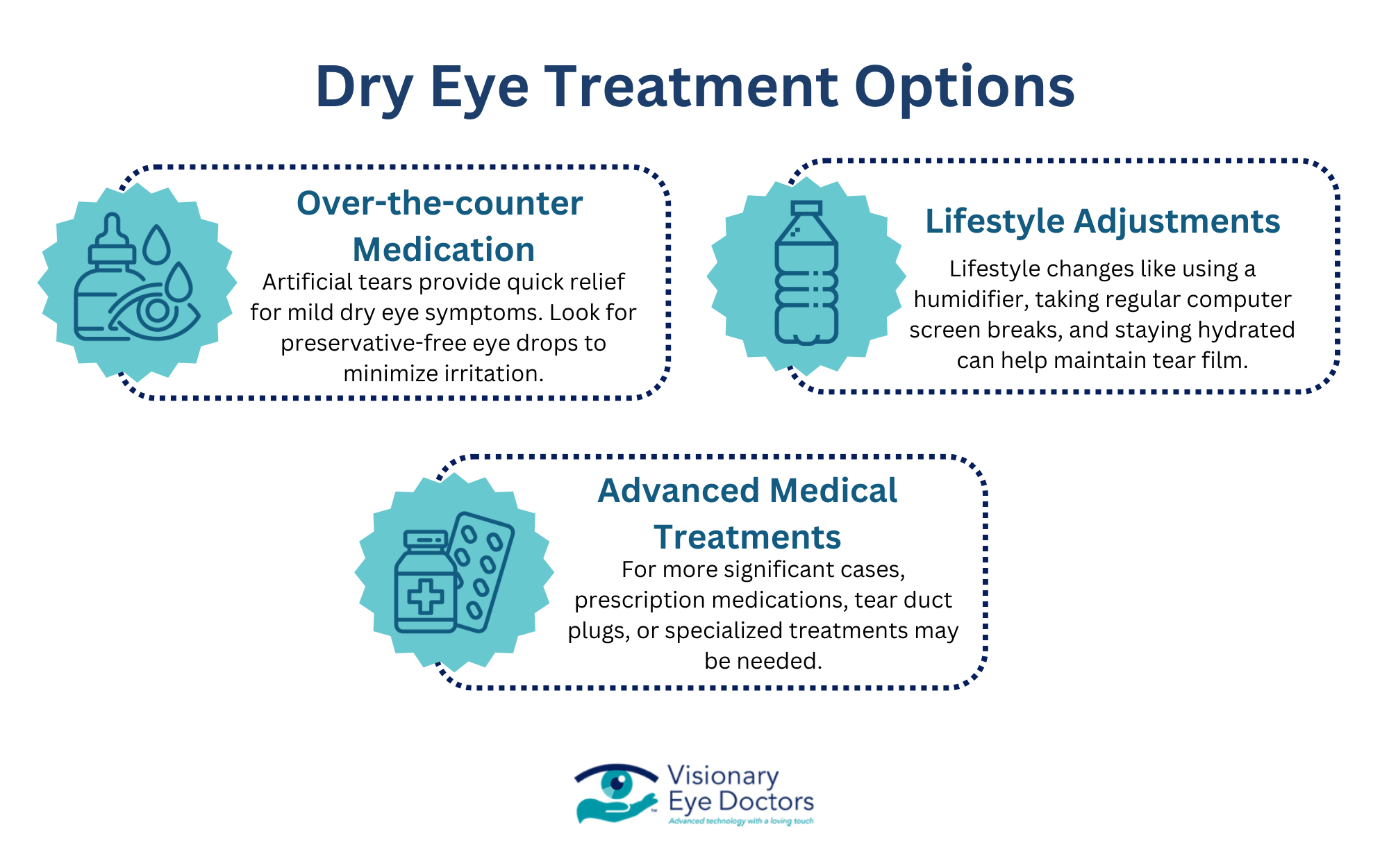
Non-Surgical Management
In mild cases, especially during the early stages, symptoms can often be managed through:
- Updated lens prescriptions
- Anti-glare coatings on glasses
- Brighter lighting at home
- Use of magnifiers or visual aids

Cataract Surgery
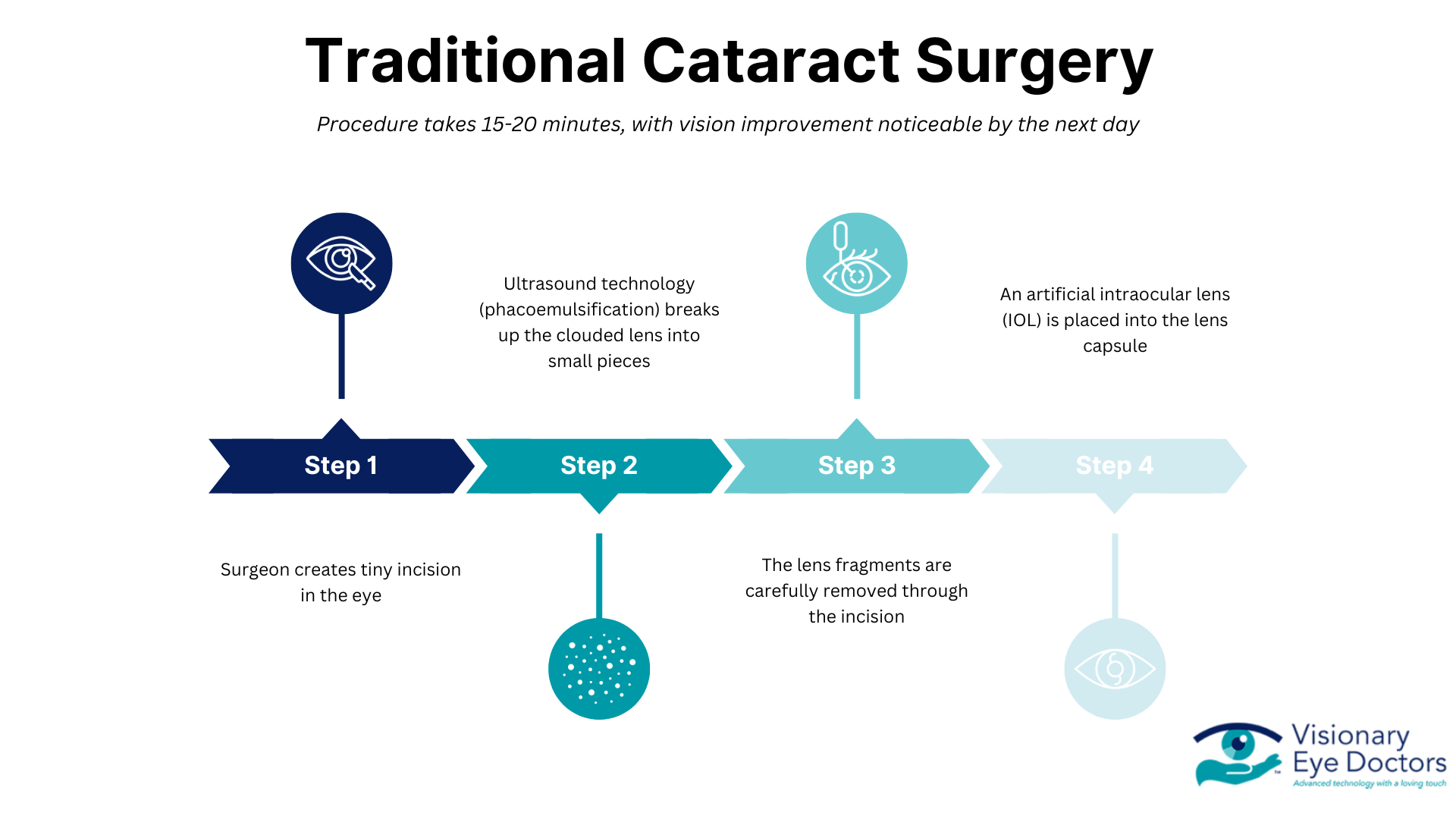
If the cataract significantly impacts your vision and daily activities, cataract surgery is recommended. This involves removing the cloudy lens and replacing it with an artificial lens, also known as an intraocular lens (IOL).
Types of IOLs include:
- Monofocal lenses – Set to focus at one distance (usually for distance vision)
- Multifocal lenses – Allow both near and far focusing
- Toric lenses – Correct astigmatism during surgery
- Light – Adjustable Lenses
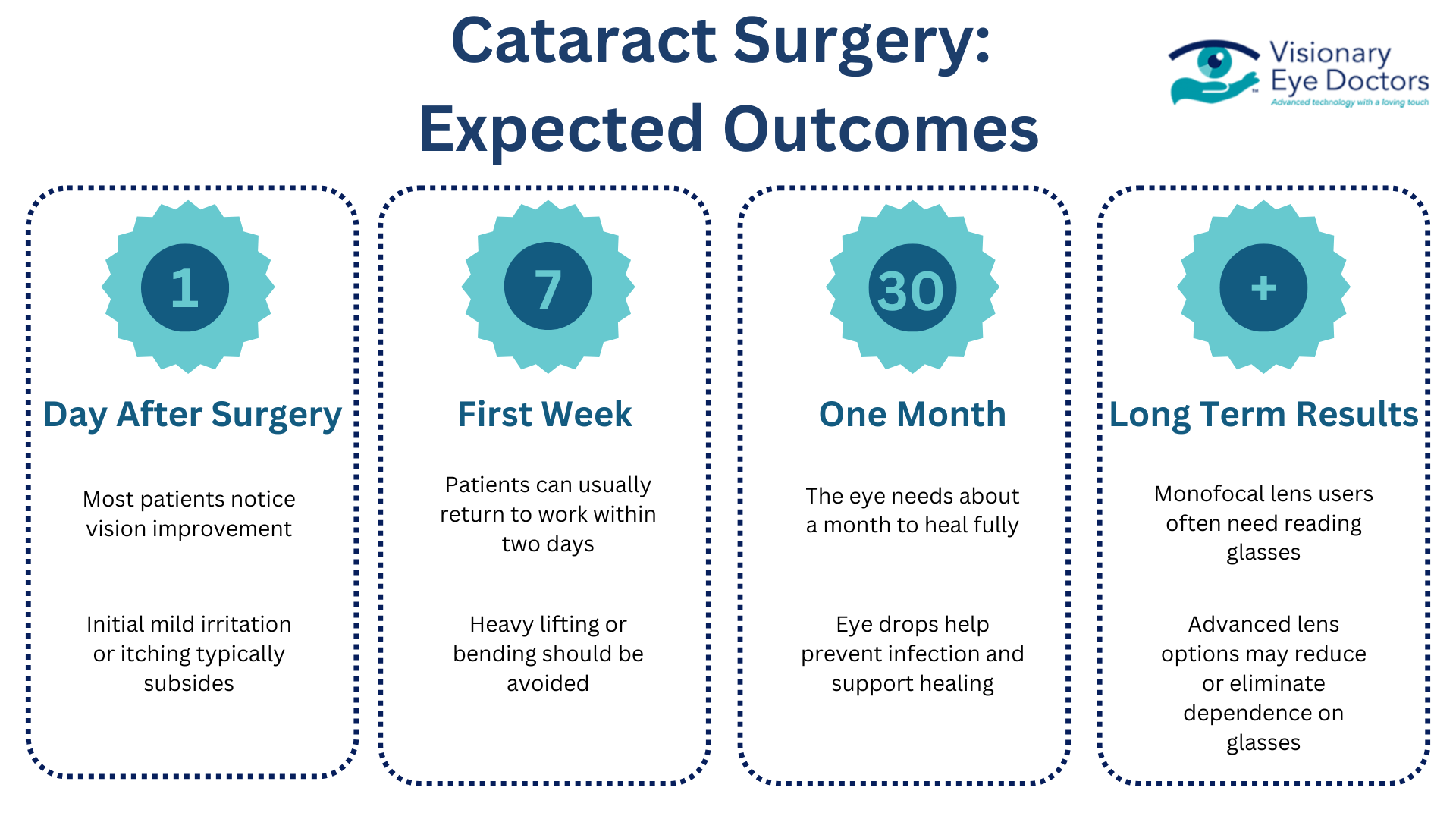
Most cataract patients report noticeable improvement in clear vision within a few days, with full recovery in 4–6 weeks.
Cataract surgery is one of the most commonly performed surgical procedures worldwide, with a success rate of over 95%. The procedure typically takes less than 30 minutes and is performed on an outpatient basis, meaning you can go home the same day. Modern techniques use ultrasound (phacoemulsification) to break up the cloudy lens before removal, requiring only tiny incisions that often heal without stitches.
Preventing Cataracts or Delaying Their Progression
While not all cataracts can be prevented, you can lower your risk by protecting your eyes and maintaining overall health:
- Wear UV-blocking sunglasses in bright conditions
- Stop smoking
- Control diabetes and other chronic illnesses
- Eat a balanced diet rich in leafy greens and antioxidants
- Follow regular exam schedules recommended by the National Eye Institute
Certain nutrients may help protect against cataract formation. Vitamins C and E, lutein, zeaxanthin, and omega-3 fatty acids have shown promise in some studies. A diet rich in colorful fruits and vegetables provides these protective compounds naturally.
Taking Action: Restoring Your Clear Vision
Cataracts are a common part of aging, but that doesn’t mean you have to live with cloudy vision or limited night vision. Recognizing the signs of cataracts early and discussing your options with an eye doctor can help you preserve your vision and quality of life.
At Visionary Eye Doctors in Maryland and Washington, DC, we’ve helped thousands of patients regain clear vision through expert diagnosis and advanced cataract surgery using the latest intraocular lens technology.
If you’ve noticed any changes in your vision, don’t wait. Schedule your eye exam today.