Exploring the Connection Between Dry Eyes and Headaches
Dry eyes and headaches often surface together, leading many to wonder if one causes the other. It’s not uncommon for individuals to experience the discomfort of dry, scratchy eyes followed by the onset of a headache later in the day. Could a physiological link between these common conditions explain their frequent co-occurrence?
Exploring how dry eyes can contribute to headache symptoms requires considering everything from eye strain to broader neurological connections. Understanding this connection can be crucial for those seeking relief and could offer insights into managing these conditions more effectively. By identifying and addressing the root causes, individuals can improve their quality of life and potentially reduce the frequency of both dry eyes and headaches.
Causes of Dry Eyes
Dry eye disease occurs when the eyes do not produce enough tears or when the tears evaporate too quickly. This imbalance in the tear film can be attributed to a variety of factors, each contributing to discomfort. Understanding these causes is the first step toward effective management and treatment.
Meibomian Gland Dysfunction
Most dry eye disease is due to dysfunction of the meibomian glands which are the microscopic oil glands of our eyelids. Looking at electronic screens, especially in kids, rewires the brain to decrease blink rates which leads to less oil production in these glands. Other factors that worsen Meibomian Gland Dysfunction include chronic contact lens use or certain medications like Isotretinoin (ie Accutane).
Environmental Factors
Conditions like low humidity, wind, and exposure to smoke or dry air can accelerate tear evaporation, leaving the eyes insufficiently lubricated.
Lifestyle Factors
Prolonged use of digital devices, which encourages infrequent blinking, significantly contributes to the rapid evaporation of tears. Similarly, extended periods of reading or driving can also dry out the eyes.
Health-Related Causes
Certain medical conditions such as Sjögren’s syndrome, rheumatoid arthritis, non-Hodgkin lymphoma, and thyroid diseases are known to impair tear production. Additionally, hormonal changes associated with menopause can also decrease tear secretion.
Medications
Various medications including antihistamines, decongestants, blood pressure medications, antidepressants, or Isotretinoin ( ie Accutane ) can reduce tear production, leading to symptoms of dry eyes.
Age
As we age, tear production naturally decreases. The majority of those affected by dry eyes are older adults, particularly those who are post-menopausal.
Contact Lens Wear
Long-term use of contact lenses can irritate the eyes and contribute to the drying of the tear film.
By identifying the specific causes contributing to dry eyes, individuals and healthcare providers can better target treatments and lifestyle adjustments to alleviate symptoms.
Symptoms of Dry Eyes

Dry eye syndrome presents a range of uncomfortable symptoms that can vary significantly in severity from person to person.
Eye Discomfort and Irritation
One of the most common symptoms of dry eyes is a persistent sense of irritation. Individuals may feel as if there is sand or grit in their eyes, leading to constant discomfort.
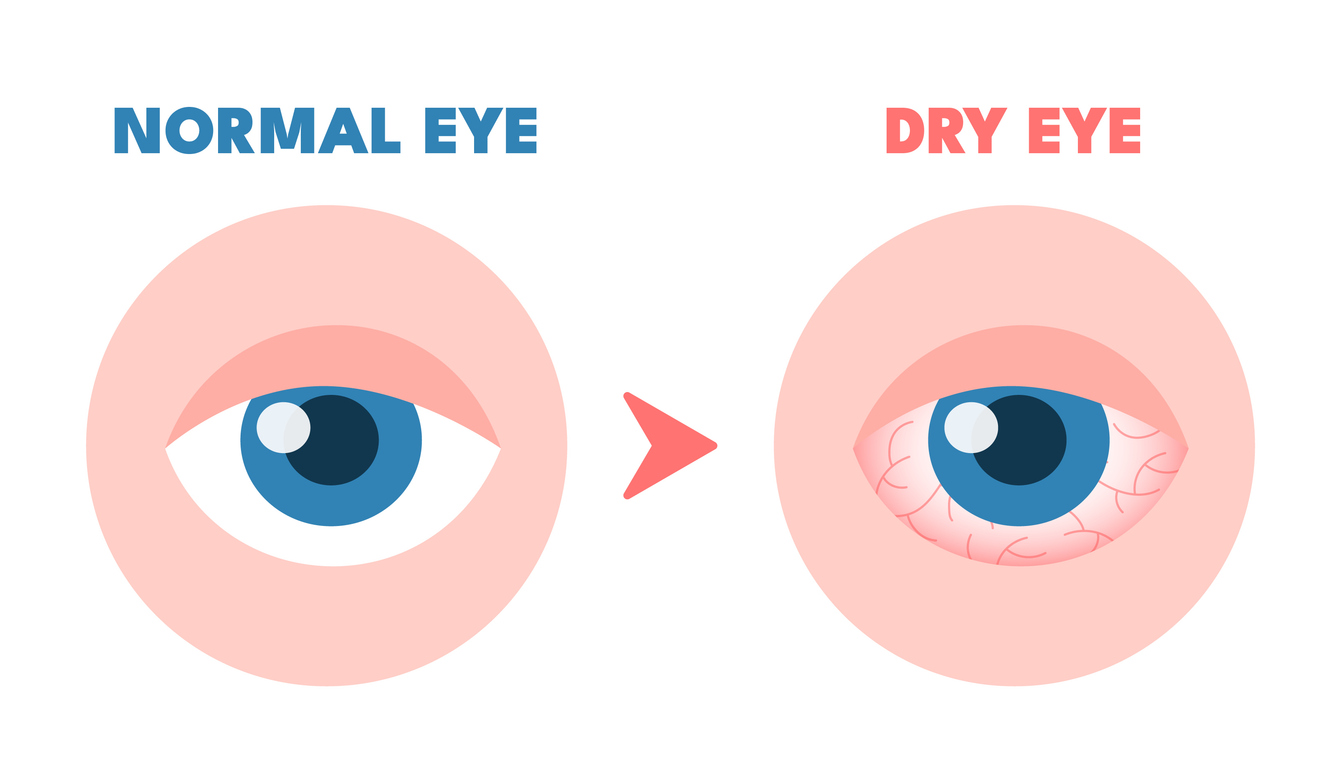
Redness
Dry eyes often look red and inflamed. The lack of adequate lubrication can cause the surface of the eye to appear more bloodshot.
Blurry Vision
Intermittent visual disturbances can occur, especially after prolonged activities that strain the eyes, such as reading or using digital screens.
Eye Fatigue
Dry eyes may feel weary or strained after only a short period of use. This can make everyday tasks that require visual focus more challenging.
Light Sensitivity
People with dry eyes might experience increased sensitivity to light, finding bright or glaring lights uncomfortable or even painful.
Excessive Tearing
Paradoxically, dry eyes can lead to episodes of excessive tearing. When the eyes are dry, they may overreact to the discomfort or irritation by producing too many tears.
Difficulty with Contact Lenses
Many individuals with dry eyes find it difficult to wear contact lenses. They may feel increased irritation or cannot keep the lenses in for their usual duration.
Understanding these symptoms helps to connect the discomfort of dry eyes with potential impacts on daily life, including the exacerbation of headaches.
How Can Dry Eyes Lead to Headaches?

The connection between dry eyes and headaches is rooted in the discomfort and strain that dry eyes can induce, which in turn can trigger headaches. Here’s a closer look at how unresolved dry eye symptoms can lead to frequent headaches:
Eye Strain
When the eyes are dry, they may not function as smoothly as they should, leading to increased effort to perform visual tasks. This additional strain can cause the muscles around the eyes and forehead to work harder, which can result in tension headaches. People who use digital devices frequently may experience this more acutely, as staring at screens can exacerbate dry eye symptoms and subsequent eye strain.
Blink Reflex
Dry eyes can disrupt the normal blinking process. Proper blinking helps maintain moisture on the eye surface by spreading tear film evenly across the eyes. However, when eyes are dry, individuals might blink more frequently or incompletely in an attempt to alleviate discomfort. This altered blinking pattern can strain the eyes further, contributing to the development of headaches.
Trigeminal Nerve Activation
The trigeminal nerve is one of the largest nerves in the head and plays a key role in transmitting sensations from the face to the brain. It also has branches that are directly involved with the eyes. When the eyes are dry and irritated, the trigeminal nerve may become overstimulated, leading to pain signals that the brain interprets as a headache. This is particularly relevant in the context of migraine headaches, where trigeminal nerve irritation is a known trigger.
Reflexive Tension
Chronic dry eye can lead to persistent discomfort, causing reflexive tensing of facial and scalp muscles. Over time, this tension can form patterns that are hard to break, even when the eyes are at rest. This ongoing muscle tension can evolve into chronic headache conditions.
Reduced Visual Quality
Dry eyes often cause blurred vision, which can lead the person to squint and strain in an attempt to see clearly. This habitual squinting and the constant effort to focus can create significant eye and head tension, manifesting as headaches.
Compounded Stress
Living with the constant irritation and discomfort of dry eyes can lead to increased stress levels. Stress is a well-known headache trigger, and managing chronic conditions like dry eye syndrome can amplify this effect, setting off a cycle where dry eyes and headaches reinforce each other.
Addressing dry eye symptoms promptly and effectively is essential not only for eye health but also for reducing the likelihood of associated headaches. For individuals experiencing both conditions, treating dry eyes might alleviate some of the headache symptoms, potentially decreasing the frequency and severity of headaches. By understanding the intricate relationship between these two conditions, patients can seek targeted treatments that offer relief for both symptoms simultaneously.
Expertise of Visionary Eye Doctors in Diagnosing and Treating Dry Eyes

At Visionary Eye Doctors, we understand the complexities of dry eye syndrome and its potential to impact not just your vision but your overall quality of life, including contributing to headaches. Led by Dr. Sandra Cremers M.D., a renowned expert in the field, our clinic is equipped with advanced diagnostic tools and treatment options tailored to address the unique needs of each patient.
We employ comprehensive diagnostic techniques to accurately assess the severity and underlying causes of your dry eye symptoms. Our approach includes the use of the SPEED™ Dry Eye Questionnaire, TearLab for osmolarity testing, and InflammaDry for detecting inflammation, among other state-of-the-art technologies. These precise diagnostics help us ensure that we are not only treating symptoms but also addressing the root cause of your dry eyes.
Recognizing that each case of dry eye is unique, we offer a variety of treatment options designed to cater to specific needs. Whether it’s through prescription artificial tears, in-office procedures like LipiFlow and IPL treatment, or recommending lifestyle changes, our goal is to provide relief that is both effective and sustainable.
We believe in empowering our patients with knowledge about their conditions. By educating about the factors contributing to dry eyes and headaches, we encourage preventive practices that can help minimize discomfort and prevent recurrence. Our team provides guidance on managing environmental factors and digital device habits, which are often crucial in controlling dry eye symptoms.
If you are frequently experiencing symptoms of dry eyes, such as irritation, redness, and blurred vision, or if these are accompanied by headaches, it’s important to seek professional help. Early intervention can prevent complications and improve your quality of life. We recommend that anyone suffering from these symptoms schedule a comprehensive eye exam to explore their treatment options.
Don’t let dry eyes and associated headaches disrupt your life—reach out to us today and take the first step towards relief.

