Is Glaucoma Hereditary? Understanding Your Family Risk
The short answer: Yes, glaucoma has a strong genetic component. If you have a family member with glaucoma, your risk increases significantly..
Glaucoma affects millions of people worldwide, damaging the optic nerve through increased intraocular pressure. This pressure builds when the eye’s drainage system doesn’t allow fluid (aqueous humor) to flow out properly. What many don’t realize is that by the time noticeable symptoms appear, permanent vision loss may have already begun.
But what exactly does this mean for you and your eye health? Let’s explore the hereditary nature of glaucoma, what it means for families, and the steps you can take to protect your vision
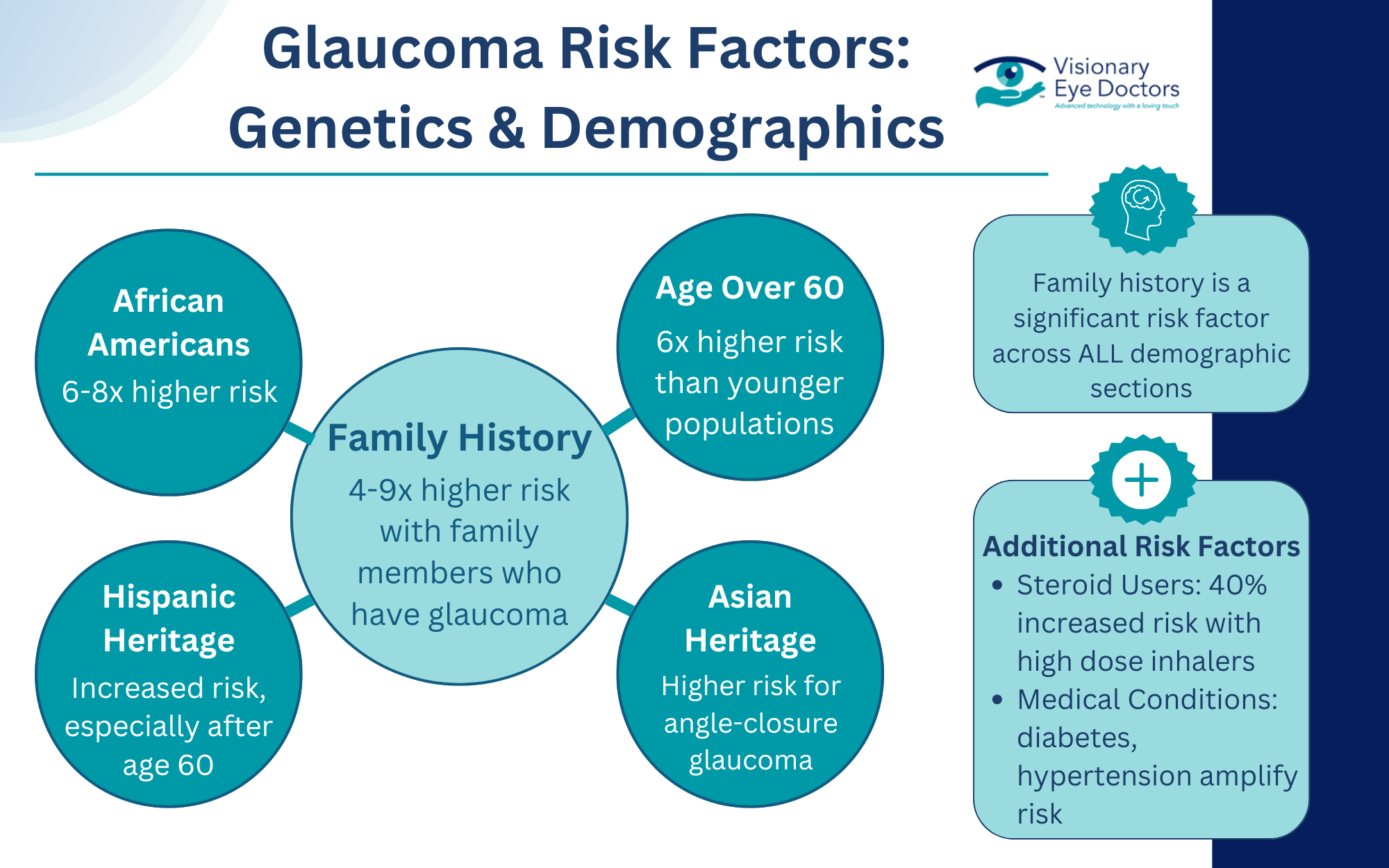
The Genetic Risk: By the Numbers
Family history stands as one of the most significant risk factors for developing glaucoma. Primary open-angle glaucoma, the most common type, has a strong genetic component that can dramatically increase your chances of experiencing optic nerve damage and potential vision loss.
When doctors know glaucoma runs in your family, they can implement more frequent screening and earlier interventions. This is crucial since intraocular pressure can damage the optic nerve without noticeable symptoms until permanent vision loss has already begun.
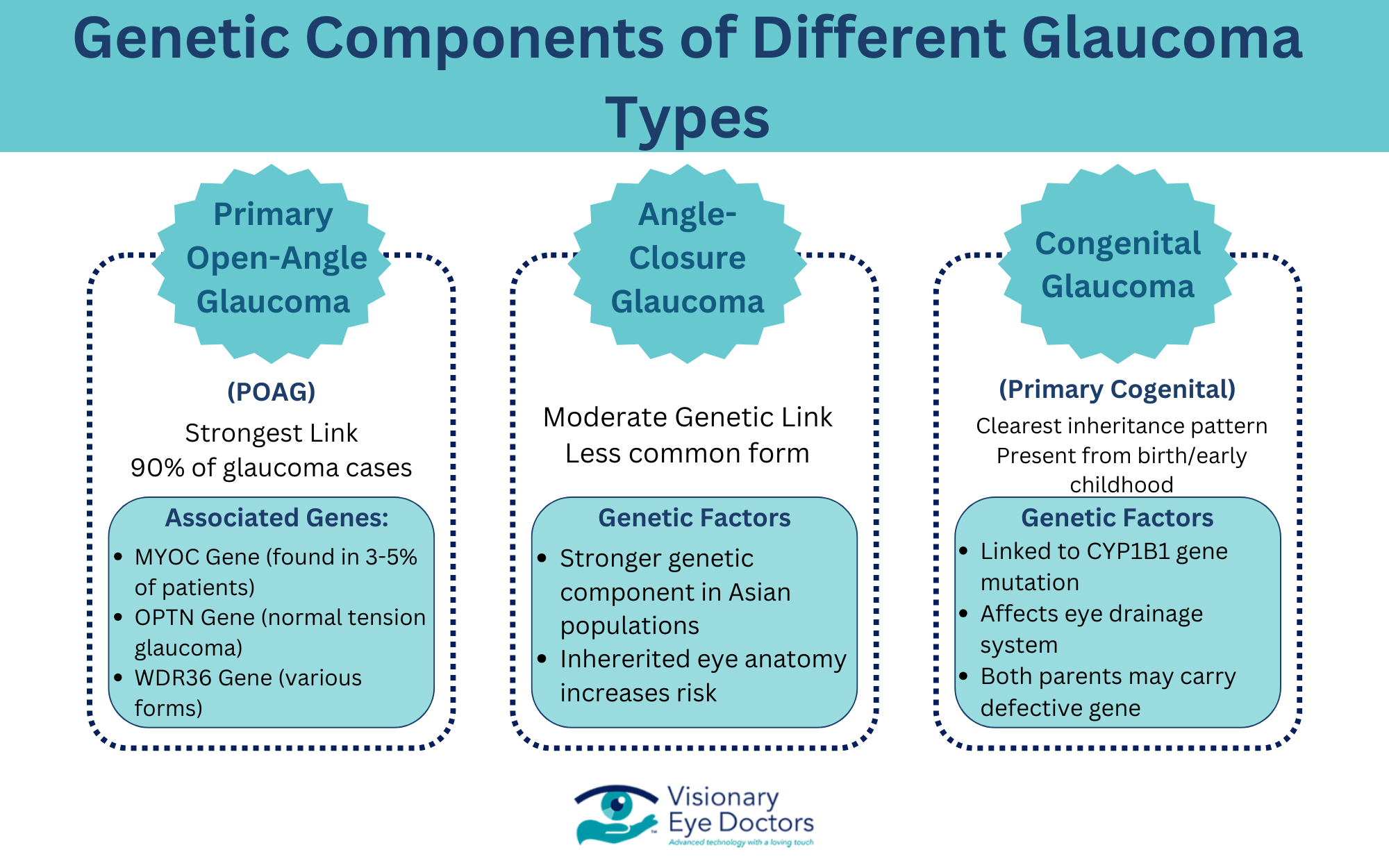
Types of Glaucoma
Not all types of glaucoma have the same genetic component. Here’s how heredity influences different forms:
Primary Open-Angle Glaucoma (POAG)
Primary open-angle glaucoma shows the strongest genetic connection. It’s the most common type, accounting for approximately 90% of all glaucoma cases in Western countries. Research has identified several specific genes linked to POAG risk, including:
- MYOC gene – Mutations here are found in 3-5% of POAG patients
- OPTN gene – Associated with normal tension glaucoma
- WDR36 gene – Linked to various forms of glaucoma
These genetic variations affect how eye pressure is regulated and how the optic nerve responds to stress. While having these genetic risk factors doesn’t guarantee you’ll develop glaucoma, it does significantly increase your likelihood.
Angle-Closure Glaucoma
Primary angle-closure glaucoma also has genetic components, particularly in certain ethnic populations. People of Asian descent have anatomical eye characteristics that can be inherited and increase the risk for this type, which can cause rapid pressure buildup and require immediate medical attention.
Congenital Glaucoma
Primary congenital glaucoma, present at birth or developing in early childhood, has the clearest inheritance pattern. This rare form is linked to mutations in the CYP1B1 gene, which affects how the eye’s drainage system develops. In many cases, both parents must carry the defective gene for a child to develop this type.
Beyond Genes: Other Risk Factors For Developing Glaucoma
While genetic predisposition creates your baseline risk, several other factors influence whether someone with a family history actually develops glaucoma:
Age
Age remains a significant risk factor for most types of glaucoma:
- Under 40: Lower risk (except with strong genetic factors)
- Ages 40-60: Moderate and increasing risk
- Over 60: Highest risk, with rates four times higher than younger populations
For those with a family history, the risk curve shifts earlier, with symptoms sometimes appearing 10-15 years sooner than in the general population.
Other Medical Conditions
Several health conditions can interact with genetic factors to further increase glaucoma risk:
- Diabetes doubles the chance of developing glaucoma and can accelerate progression
- Hypertension affects blood flow to the optic nerve
- Heart disease may compromise oxygen delivery to eye tissues
- Sleep apnea has been linked to normal tension glaucoma
- Managing these conditions becomes especially important for those with a family history of glaucoma.
Environmental Factors and Lifestyle
Even with genetic risk factors, lifestyle choices can help reduce your overall risk:
- Regular exercise can help maintain healthy eye pressure levels
- Smoking cessation improves blood vessel health and oxygen flow
- Eye protection prevents injuries that could trigger secondary glaucoma
- Limited steroid use (when medically appropriate) reduces medication-induced pressure increases
- Proper hydration supports overall eye health

Family History: What You Need to Know and Share
Understanding your family’s eye health history can help you and your eye doctors be proactive when it comes to glaucoma development. Consider these questions:
- Has anyone in your immediate family been diagnosed with glaucoma?
- At what age did their glaucoma develop?
- What type of glaucoma do they have?
- How severe is their condition?
- What treatments have they needed?
Create a basic family eye health tree extending to grandparents, parents, siblings, and children. Share this information with your eye doctor to help them determine your risk level and appropriate screening schedule.
Testing and Early Detection: Your Prevention Strategy
For those with a family history of glaucoma, early and regular screening becomes vital. While genetic testing can provide additional information in some cases, comprehensive eye exams remain the primary tool for detection.
When to Start Regular Screenings
If glaucoma runs in your family, follow these guidelines:
| Age Group | Family History | Recommended Screening Frequency |
| Under 40 | Yes | Every 1-2 years |
| 40-54 | Yes | Annually |
| 55+ | Yes | Every 6-12 months |
| Any Age | No | Every 2-4 years (more frequently after 40) |
What to Expect During a Comprehensive Eye Exam
During a comprehensive eye exam for glaucoma, your doctor will perform several key tests to assess your eye health. The process begins with tonometry to measure intraocular pressure, followed by visual field testing to check your peripheral vision for any early signs of vision loss. Your doctor will then conduct a dilated eye examination, which allows for a thorough inspection of the optic nerve to detect any signs of optic nerve damage.
For more detailed evaluation, optical coherence tomography (OCT) creates precise images of your optic nerve structure, helping identify subtle changes that might indicate glaucoma. Finally, pachymetry measures your corneal thickness, as thinner corneas can increase glaucoma risk. These non-invasive tests provide a complete picture of your eye health, making regular eye exams essential for early detection and preventing permanent vision loss.
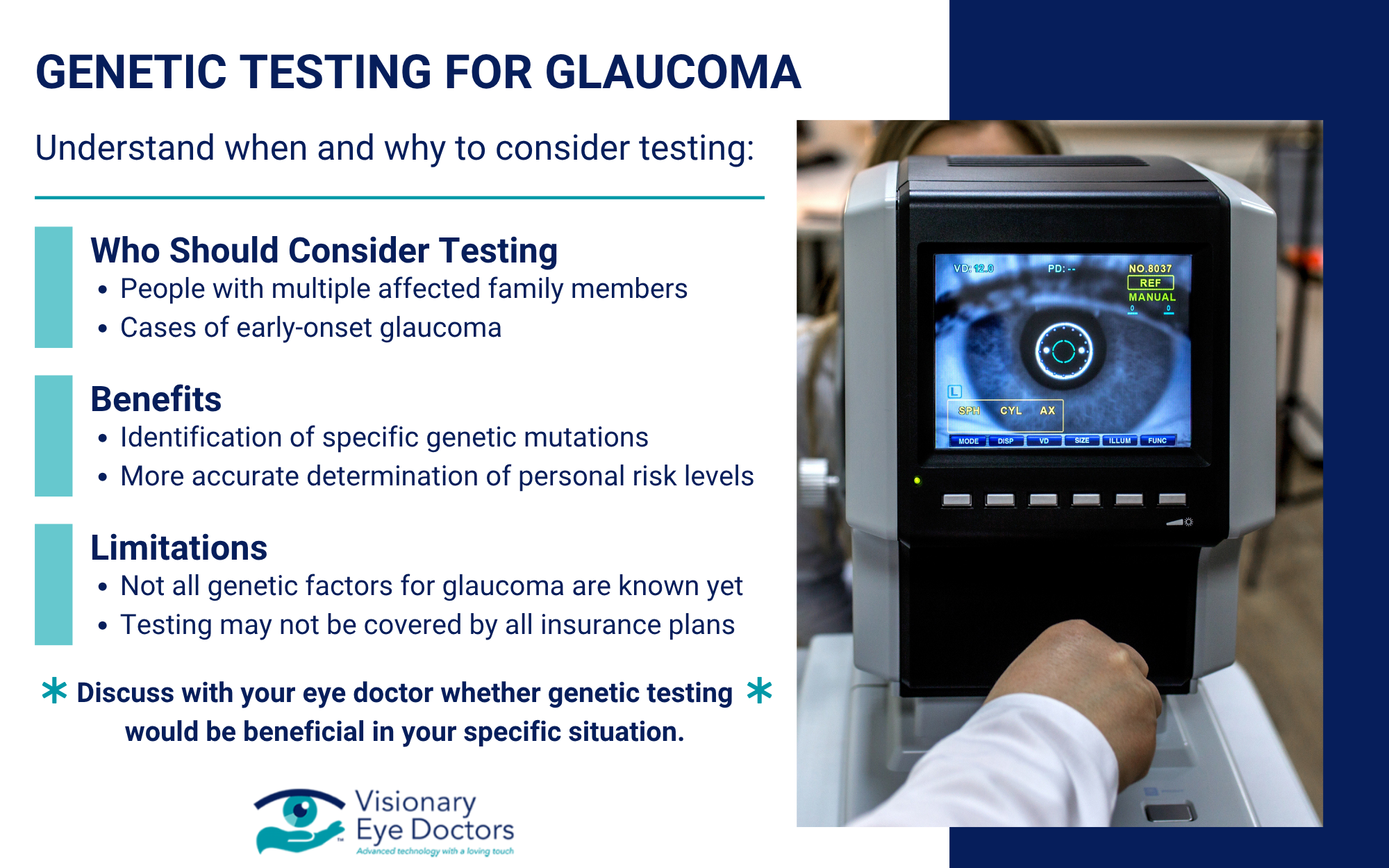
Genetic Testing Options
For families with strong patterns of glaucoma, genetic testing offers valuable insights into your risk profile. This testing benefits those with multiple affected family members, early-onset glaucoma, or rare disease forms by identifying specific mutations and determining personal risk levels. While the process requires just a simple blood or saliva sample, it’s important to note that not all genetic factors for glaucoma are known yet. Discuss with your eye doctor whether this testing would be beneficial for your specific situation.
Proactive Steps to Minimize Glaucoma Risks
If your family history puts you at higher risk for glaucoma, taking proactive steps becomes essential:
Monitor Your Eye Health
- Keep regular appointments with your eye doctor
- Know your baseline numbers for eye pressure and visual field tests
- Watch for warning signs between examinations
Know the Warning Signs
While early-stage glaucoma often lacks noticeable symptoms, be alert for:
- Gradual loss of peripheral vision
- Seeing halos around lights
- Eye pain or severe headaches (especially with closed-angle glaucoma)
- Redness in the eye
- Vision changes that don’t improve
Contact your eye doctor immediately if you experience sudden vision changes or eye pain, as these could indicate acute angle-closure glaucoma requiring urgent care.

Treatment Options: Early Intervention Matters
For those diagnosed with glaucoma, treatment options typically include:
- Eye drops to lower intraocular pressure
- Laser treatments to improve drainage
- Minimally invasive glaucoma surgeries (MIGS)
- Traditional surgeries like trabeculectomy for advanced cases
The key is early diagnosis, which allows for less invasive treatments and better vision preservation. This is particularly important for those with genetic risk factors, who may see more rapid progression without intervention.
Knowledge is Protection
Understanding the genetic component of glaucoma empowers you to take control of your eye health. While you can’t change your genetic makeup, knowing your family history allows you to work closely with eye care professionals to detect and manage glaucoma early, when it matters most.
At Visionary Eye Doctors, we specialize in comprehensive glaucoma care, from advanced diagnostics to the latest treatment options. We encourage everyone, especially those with a family history of glaucoma, to schedule regular comprehensive eye exams.
Don’t wait until vision changes occur. Take this proactive step today by contacting us to schedule an appointment. Your vision is precious – let us help you protect it.



