Botox® vs Fillers: Which Treatment is Right for You?
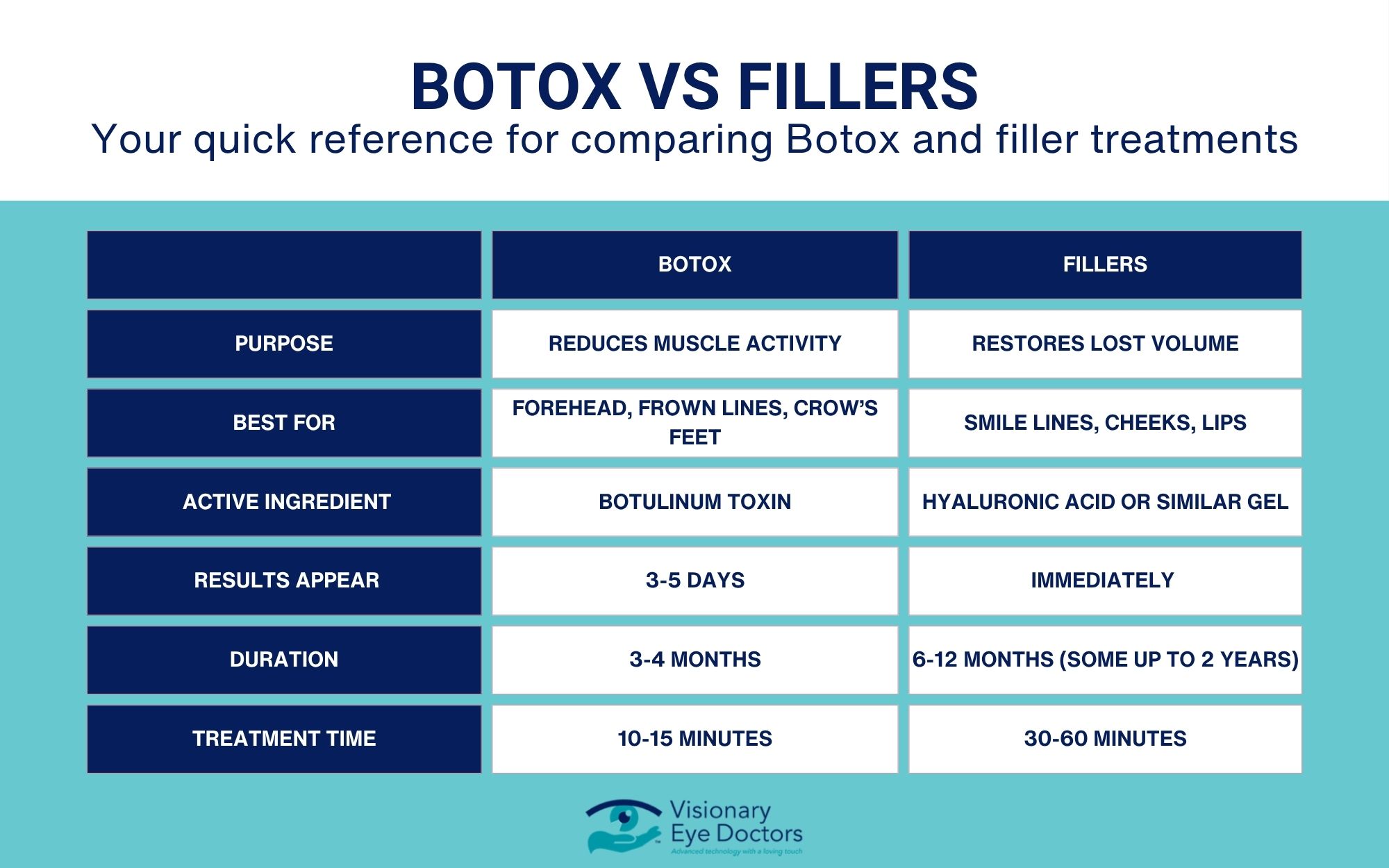
The Short Answer: Botox® works by relaxing facial muscles to reduce dynamic wrinkles caused by facial expressions, while dermal fillers add volume to smooth static wrinkles and restore facial features. Botox contains botulinum toxin that temporarily blocks nerve signals to muscles, whereas fillers use gel-like substances such as hyaluronic acid to plump and fill areas of volume loss.
Both are effective cosmetic treatments, but they work in different ways to achieve a revitalized appearance. Understanding the difference between these injectable treatments helps you choose the right option for your aesthetic goals.
At Visionary Eye Doctors, Dr. Mahan, a Botox expert, specializes in advanced techniques and is well-known for training other physicians in these methods, including the Botox brow lift, which elevates the brows and makes the eyes appear more open and refreshed. Her expertise ensures that you receive the best care possible to achieve natural, lasting results.
Botox
What Is Botox?
Botox is an injectable treatment derived from bacterium clostridium botulinum. It’s a cosmetic procedure that temporarily relaxes facial muscles to reduce the appearance of wrinkles caused by repeated muscle movement.
When you make facial expressions like smiling, frowning, or squinting, your facial muscles contract and create lines on your skin. Over time, these dynamic wrinkles become more pronounced.
How Does Botox Treatment Work?
Botox injections work by blocking nerve signals to specific facial muscles. When interrupted, the targeted muscles can’t contract as forcefully. This muscle relaxation smooths out the skin above, reducing the appearance of wrinkles and fine lines.
The effects of Botox typically appear within a few days and last three to six months.
Common Treatment Areas for Botox
Botox is most effective for treating dynamic wrinkles in the upper face:
- Forehead lines: Horizontal lines across the forehead caused by raising your eyebrows
- Frown lines: Vertical lines between the eyebrows
- Crow’s feet: Fine lines that radiate from the outer corners of your eyes
- Forehead wrinkles: Expression lines that deepen with repeated facial movements
Botox can also be used for the lower face: marionette lines (downturned mouth), TMJ/masseter (good for jaw clenching and also slimming of the jaw line), chin dimpling, “lip flip”
Dr. Mahan also performs botox injections for medical conditions including TMJ dysfunction, facial spasms, blepharospasm, myokymia, and migraine. Some of these treatments may be covered by insurance.
What to Expect During Treatment
A botox injection session typically takes just 10-15 minutes. Your healthcare provider will use a fine needle to inject small amounts of botulinum toxin into specific facial muscles. Most people describe the sensation as a slight pinch at the injection site. No anesthesia is usually needed, and you can return to normal activities immediately.
Potential Side Effects
People can experience minimal side effects from Botox treatment:
- Mild bruising or swelling at the injection site
- Headache (usually resolves within 24-48 hours)
- Temporary drooping of the eyelid (rare)
- Flu-like symptoms (uncommon)
Serious side effects are rare when administered by a board-certified surgeon.
Dermal Fillers
What Are Dermal Fillers?
Dermal fillers are gel-like substances injected beneath the skin to restore lost volume, smooth wrinkles, and enhance facial features. Unlike Botox, which works on muscle movement, facial fillers physically fill in areas where volume has decreased due to aging.
Dermal filler injections can plump thin lips, soften facial creases, and improve the appearance of static wrinkles.
Types of Fillers
Different types of fillers serve different purposes:
- Hyaluronic acid fillers: The most popular type. Hyaluronic acid is a naturally occurring substance in your body that helps skin retain moisture. These provide natural-looking results and can be reversed if needed. Dr. Mahan exclusively uses hyaluronic acid fillers due to their excellent safety profile and reversibility.
- Calcium hydroxylapatite: A heavier filler used for deeper wrinkles and facial contouring.
- Poly-l-lactic acid: Stimulates your skin to produce more collagen gradually, with results lasting up to two years.
Common Treatment Areas for Fillers
Dermal filler injections are most effective for static wrinkles and volume loss:
- Smile lines: Lines running from the sides of your nose to the corners of your mouth
- Marionette lines: Lines extending downward from the corners of your mouth
- Lips: Add volume and define the lip border
- Cheeks: Restore volume loss for a more youthful appearance
- Under-eye area: Fill hollow areas to reduce a tired appearance
- Temple: fill hollow temples that contribute to aged appearance
What to Expect During Treatment
A dermal filler injection session typically takes 30-60 minutes. Your plastic surgeon or dermatologist may apply numbing cream before injections. Many modern fillers also contain lidocaine for added comfort during the cosmetic treatment.
Results are visible immediately, though some swelling may temporarily mask the final outcome.
Potential Side Effects
Most side effects from dermal filler injections are mild and temporary:
- Swelling and bruising at the injection site
- Redness or tenderness in treated areas
- Lumps or bumps under the skin (usually temporary)
- Allergic reaction (rare, especially with hyaluronic acid fillers)
Serious complications are uncommon when performed by an experienced healthcare provider. Your surgeon will discuss these risks with you at the time of your consultation.
Botox vs Fillers: Key Differences
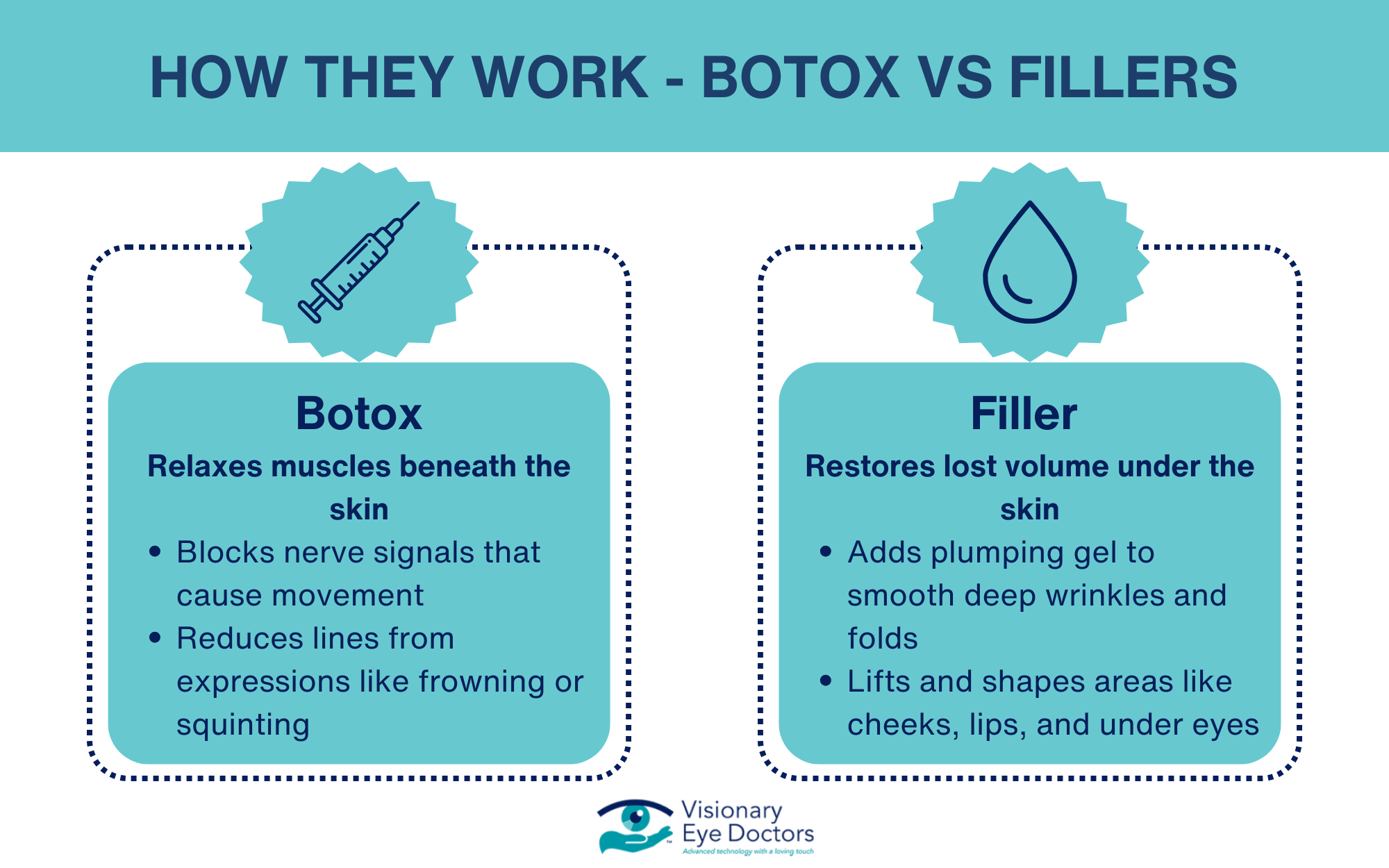
How They Work
Botox temporarily weakens facial muscles to prevent dynamic wrinkles caused by facial movements. It doesn’t add volume but prevents wrinkle formation through muscle relaxation.
Fillers physically fill spaces beneath the skin to add volume and smooth static wrinkles. They don’t affect muscle movement but restore fullness to areas with volume loss.
Treatment Areas
Botox is most effective for the upper face, including forehead lines, frown lines, and crow’s feet caused by repeated facial expressions.
Fillers work best for the mid and lower face, such as smile lines, marionette lines, lips, and cheeks where volume restoration is needed.
Duration of Results
Botox effects typically last three to six months. Regular botox treatment maintains results.
Filler duration varies by type. Hyaluronic acid fillers last six to twelve months, while poly-l-lactic acid can last up to two years.
Can You Use Both Treatments?
Yes! Many people combine Botox and fillers in different ways to achieve complete facial rejuvenation:
- Botox for forehead wrinkles and crow’s feet
- Fillers for smile lines and volume loss in cheeks
- A customized treatment plan addressing multiple concerns
Combining these cosmetic treatments creates balanced, natural-looking results that address both dynamic and static wrinkles.
Choosing the Right Treatment for Your Goals
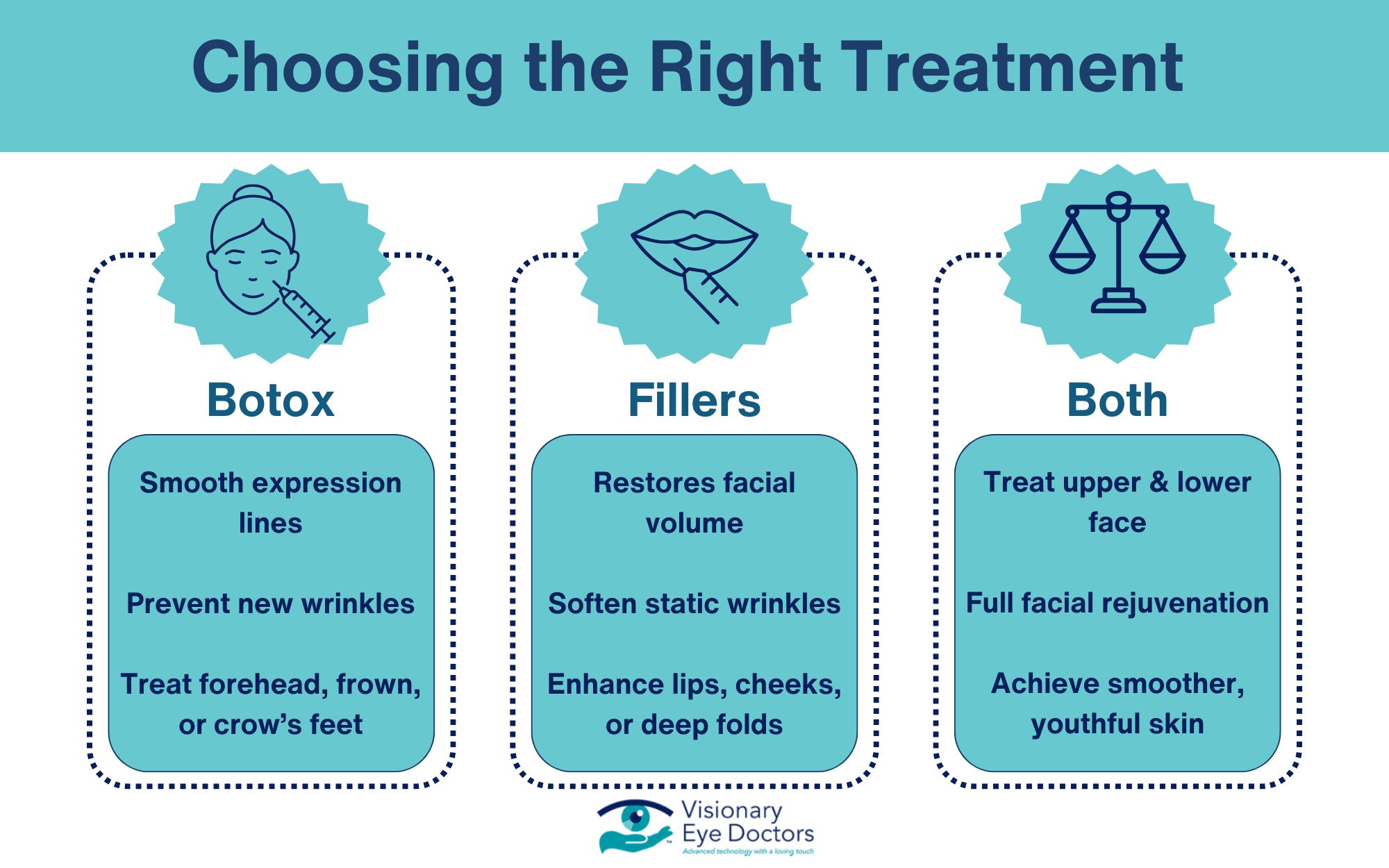
Choose Botox if you want to:
- Reduce wrinkles caused by facial expressions
- Prevent new fine lines from forming
- Smooth forehead lines, frown lines, or crow’s feet
Choose fillers if you want to:
- Restore volume to areas of your face
- Smooth wrinkles visible even at rest
- Enhance lips or cheeks
- Fill deep creases like smile lines or marionette lines
Consider both treatments if you want:
- Balanced facial rejuvenation
- To address concerns in both upper and lower face
- Maximum improvement in your healthier-looking skin
Finding the Right Provider
Choosing a qualified healthcare provider is important for safe, effective results. Look for a board-certified dermatologist or plastic surgeon with extensive experience in injectable treatments.
At Visionary Eye Doctors, our oculofacial plastic surgery team specializes in treatments for the delicate eye area and upper face. We understand the unique anatomy around the eyes and can help you achieve natural-looking results while prioritizing your safety and satisfaction.
Your Path to a More Youthfull Appearance

Both Botox and dermal fillers are proven, effective cosmetic treatments that can help you achieve your aesthetic goals. Whether you’re concerned about dynamic wrinkles from facial expressions or static wrinkles from volume loss, these injectable treatments offer safe solutions to smooth wrinkles and restore facial features.
The key is getting an accurate assessment from a qualified healthcare provider who can recommend the right cosmetic procedure for your individual needs. Some people benefit from Botox alone, others from fillers alone, and many find that combining both treatments provides the most comprehensive results.
Don’t let concerns about facial wrinkles or fine lines affect your confidence. Modern injectable treatments, administered by experienced professionals, help you maintain a natural, youthful appearance while preserving your unique facial movements.
Schedule a consultation with the oculofacial plastic surgery specialists at Visionary Eye Doctors to discuss whether Botox, fillers, or a combination of both is right for you. With the right cosmetic treatment plan, you can achieve the refreshed, radiant look you desire.