If I Stop Drinking Coffee Will That Help With Glaucoma?
Reducing or stopping coffee consumption may influence glaucoma, as caffeine can temporarily raise intraocular pressure (IOP) – a key factor in glaucoma risk. However, the impact varies based on several factors such as genetic predisposition, caffeine sensitivity, and overall eye health.
Understanding the role that caffeine has in your eye health demonstrates the importance of consulting an eye doctor for personalized guidance specific to your needs.
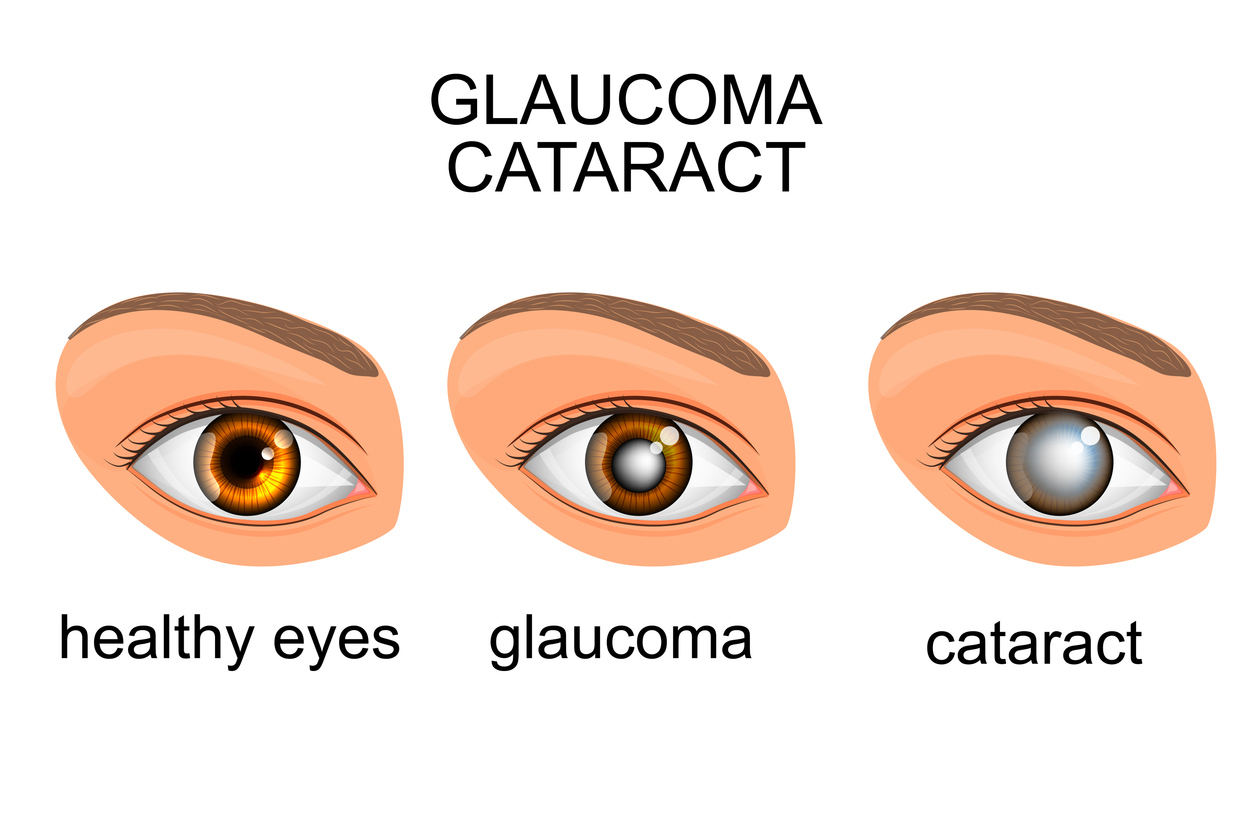
What is Glaucoma and What are the Risk Factors?
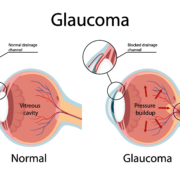
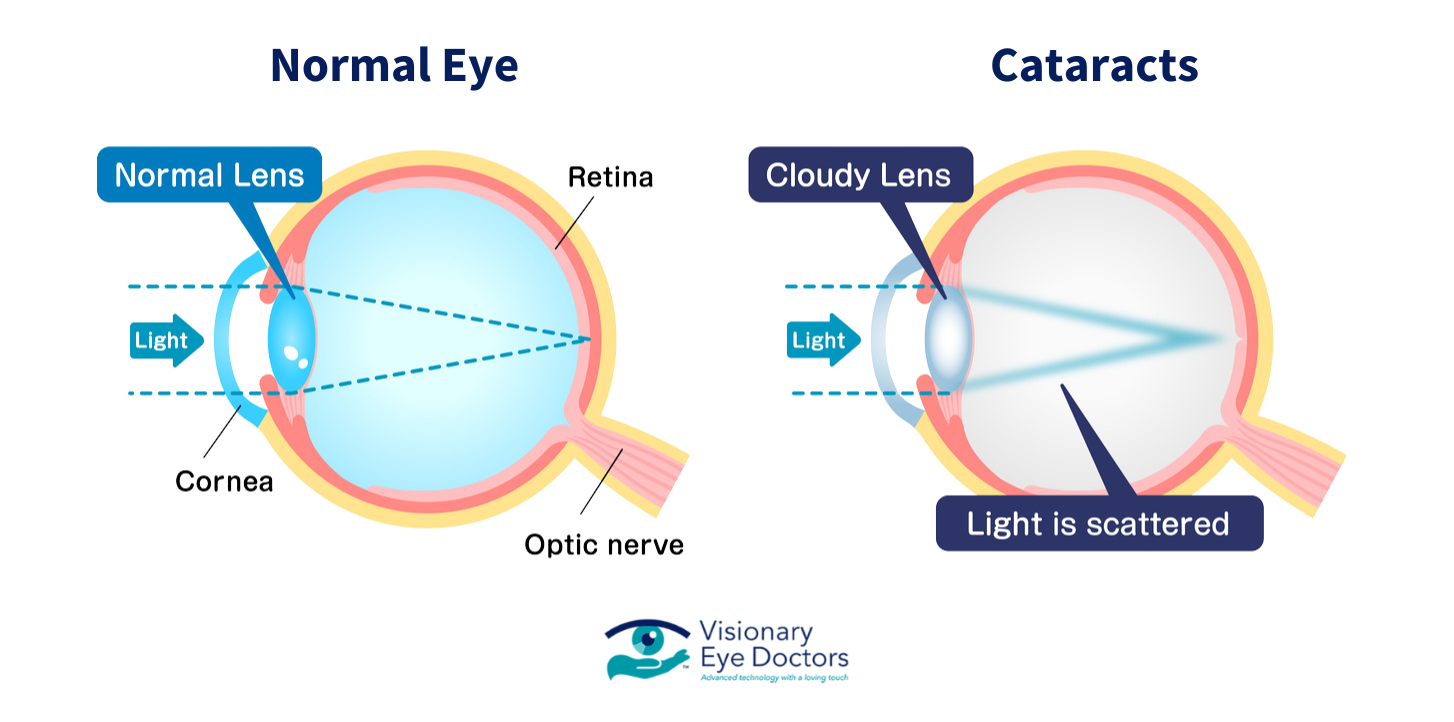
Glaucoma is an eye disease that damages the optic nerve, which is essential for transmitting visual information from the eye to the brain. This damage is often caused by increased intraocular pressure, a condition that occurs when build builds up in the eye. Over time, untreated glaucoma can lead to permanent vision loss or blindness.
While not all glaucoma cases involve high IOP, managing eye pressure remains a key part of preventing optic nerve damage.
Types of Glaucoma
- Open-Angle Glaucoma: The most common form, this condition develops gradually as the drainage angle in the eye remains open but becomes less efficient over time. Symptoms are often unnoticed in its early stages, making regular eye exams crucial.
- Acute-Closure Glaucoma: Less common, but causes a sudden build-up of pressure in the eye because the drainage angle is too narrow.
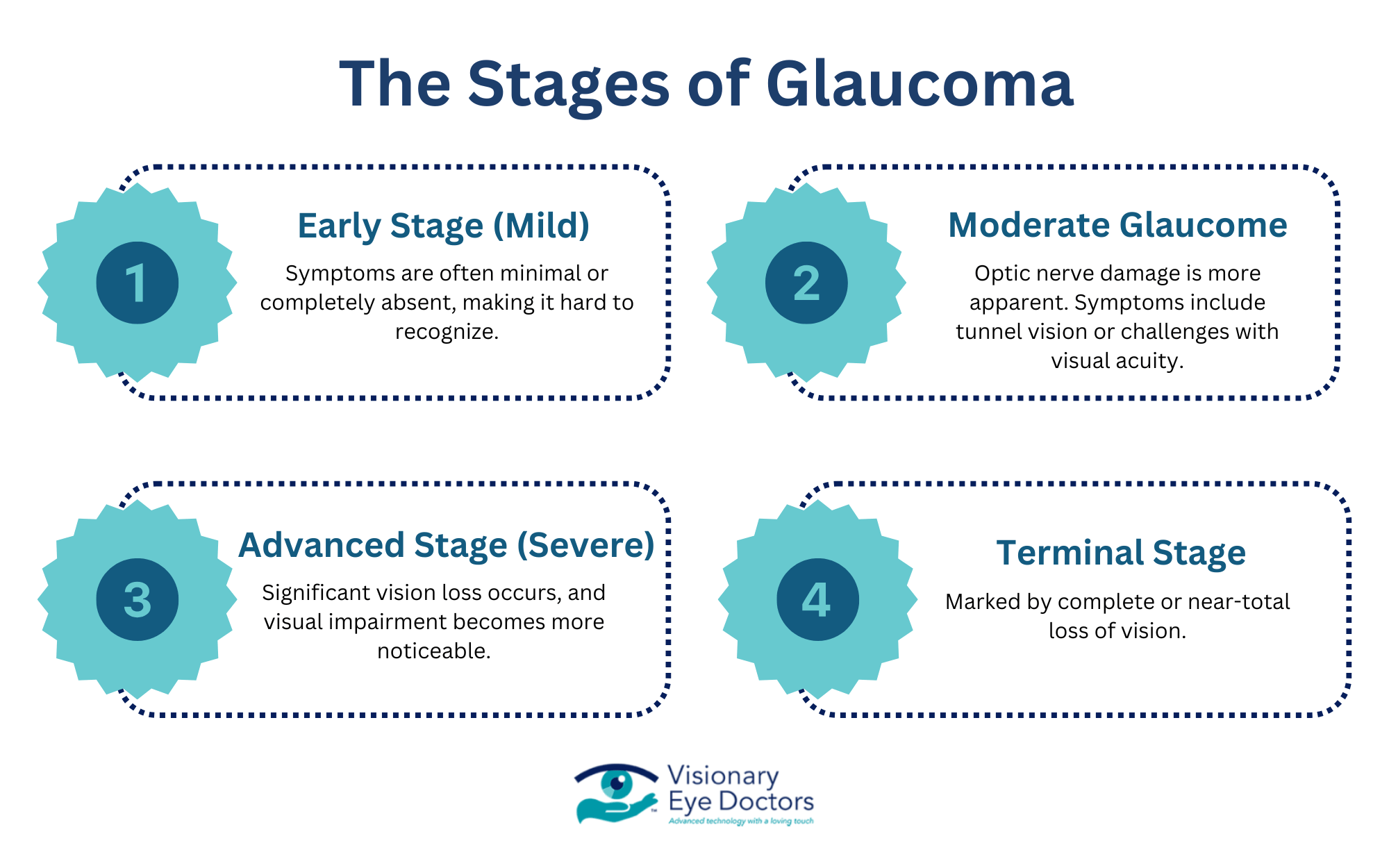
Without timely intervention, glaucoma progresses to advanced stages, potentially leading to significant vision loss and even blindness.
Factors Contributing to Glaucoma Risk
Genetic Predisposition
A family history of glaucoma significantly increases your risk. If a parent or sibling has been diagnosed with the condition, regular screenings are essential to detect early changes in your eye health.
Lifestyle Choices
Caffeine consumption and alcohol intake may contribute to changes in IOP. While caffeine can cause a temporary increase in eye pressure, its long-term effects vary from person to person. Moderating these habits can support overall eye health.
Co-Occurring Conditions
Conditions like diabetic retinopathy and macular degeneration can even compound the risk of glaucoma. Managing these separate conditions effectively is crucial to maintaining healthy vision and reducing the likelihood of glaucoma-related complications.
By understanding these risk factors and maintaining regular eye exams, you can take proactive steps toward protecting your eyes.
The Impact of Caffeine on Eye Pressure and Glaucoma
Caffeine, a natural stimulant found in coffee, tea, and many energy drinks, can affect eye pressure by causing a temporary spike in IOP. This occurs because caffeine may affect the drainage system in the eye, slowing the outflow of aqueous humor – the liquid inside of the front eye that regulates eye pressure. Over time, elevated IOP can put stress on the optic nerve, leading to a higher risk of glaucoma.
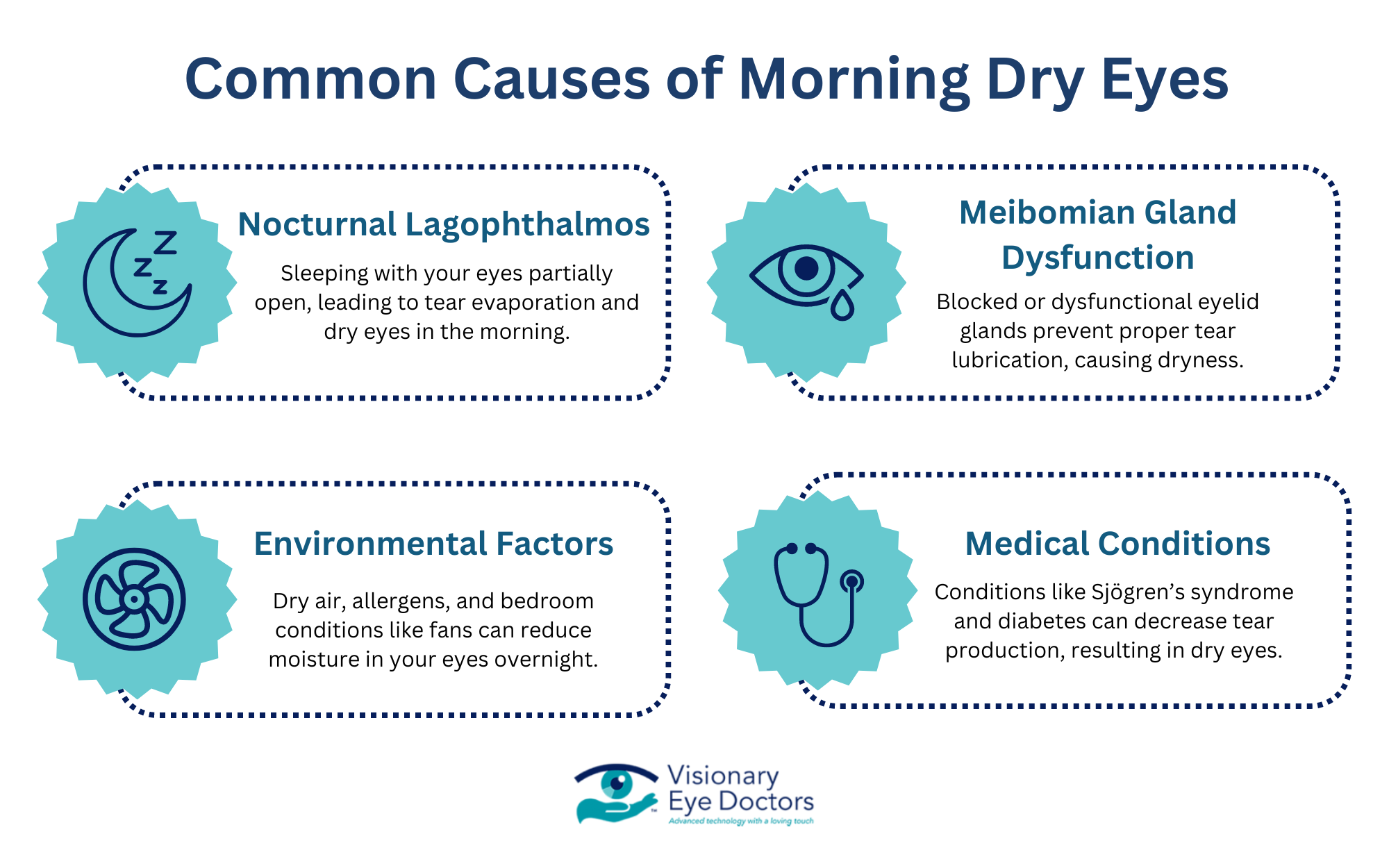
Studies have mentioned potential side effects of excessive caffeine consumption – blurry vision or dry eye – both of which impair overall visual comfort. While these effects are often temporary, they can be more extreme in individuals with pre-existing eye conditions like glaucoma.
Coffee vs. Other Caffeinated Drinks
Not all caffeinated drinks affect eye health in the same way. Coffee, which typically has higher caffeine levels per serving compared to tea or soft drinks, has been associated with more significant changes in IOP.
Energy drinks, which often combine caffeine with other stimulants, may have a greater risk for those with caffeine sensitivity.
Research suggests a potential link between regular high caffeine intake and an increased odds ratio for glaucoma. However, the exact risk can vary depending on the source of caffeine and individual tolerance levels, as well as genetic predispositions. For example:
- Coffee: Associated with more IOP changes due to higher caffeine content.
- Energy Drinks: Often combine caffeine with other additives, potentially increasing the impact on eye pressure.
- Soft Drinks and Tea: Typically have lower caffeine levels, so a milder effect on IOP.
If you’re concerned about your level of caffeine intake and how that impacts your eye health, consult with your eye doctor to discuss risk factors and how to manage them.
Lifestyle Adjustments for Glaucoma Patients
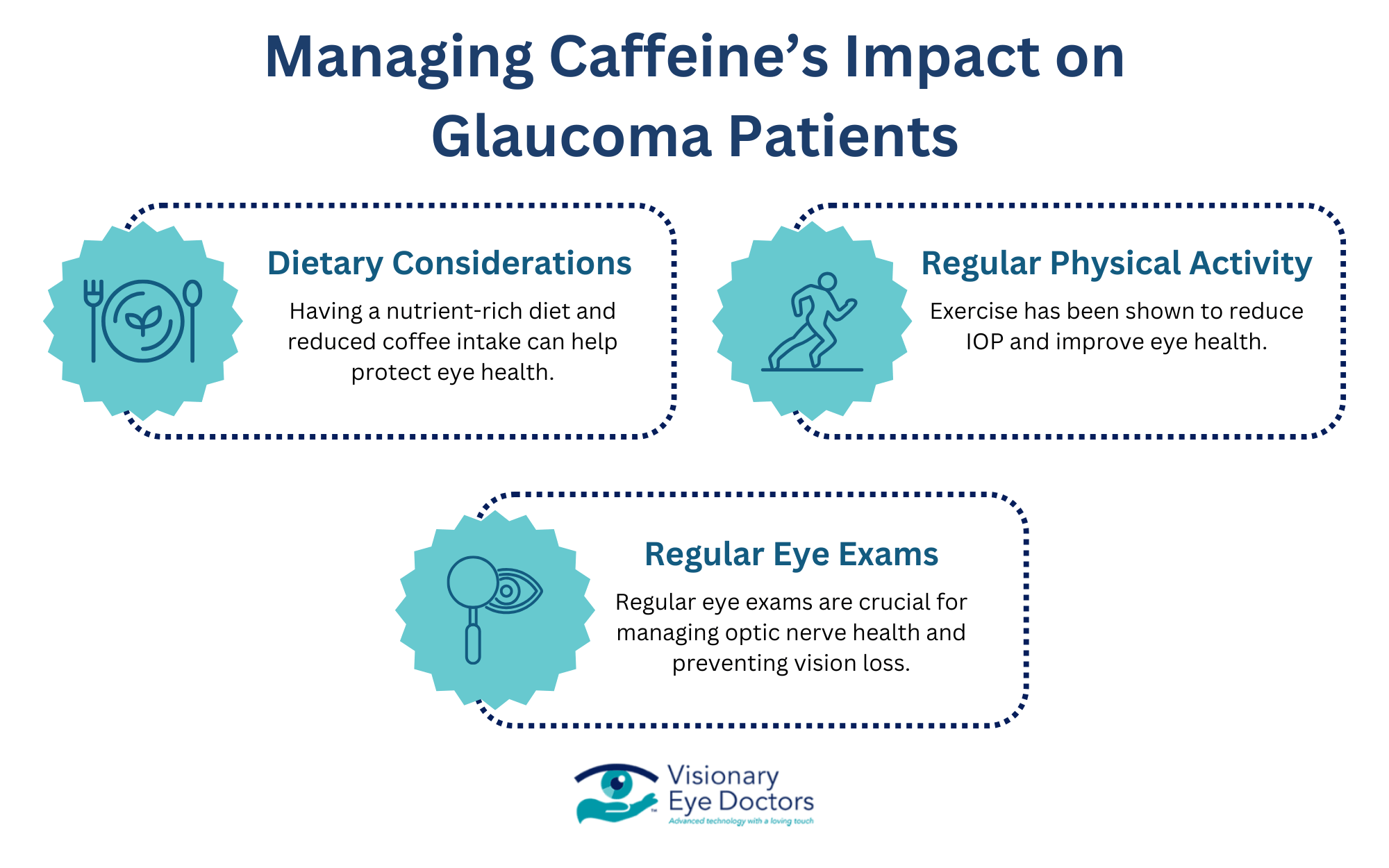
Dietary Considerations
Making mindful dietary choices can play a role in managing glaucoma and supporting overall eye health. Switching to decaf coffee or reducing regular coffee consumption may help minimize spikes in intraocular pressure, especially for those who are more sensitive to caffeine in general. Choosing decaffeinated options allows you to enjoy the taste of coffee without the potential IOP risks.
A nutrient-rich diet is another component of eye health. Incorporating green leafy vegetables – which are high in antioxidants – and omega-3 fatty acids can help protect the optic nerve and improve blood flow in the eyes.
These dietary adjustments may not only benefit people with glaucoma but also support long-term vision health.
Regular Exercise and Physical Activity
Beyond diet, regular physical activity is a key factor in managing your vision. Exercise has been shown to reduce IOP in some individuals, improving overall circulation and eye health. Activities like walking, swimming, or yoga can be a low-impact but effective way to maintain a healthy lifestyle.
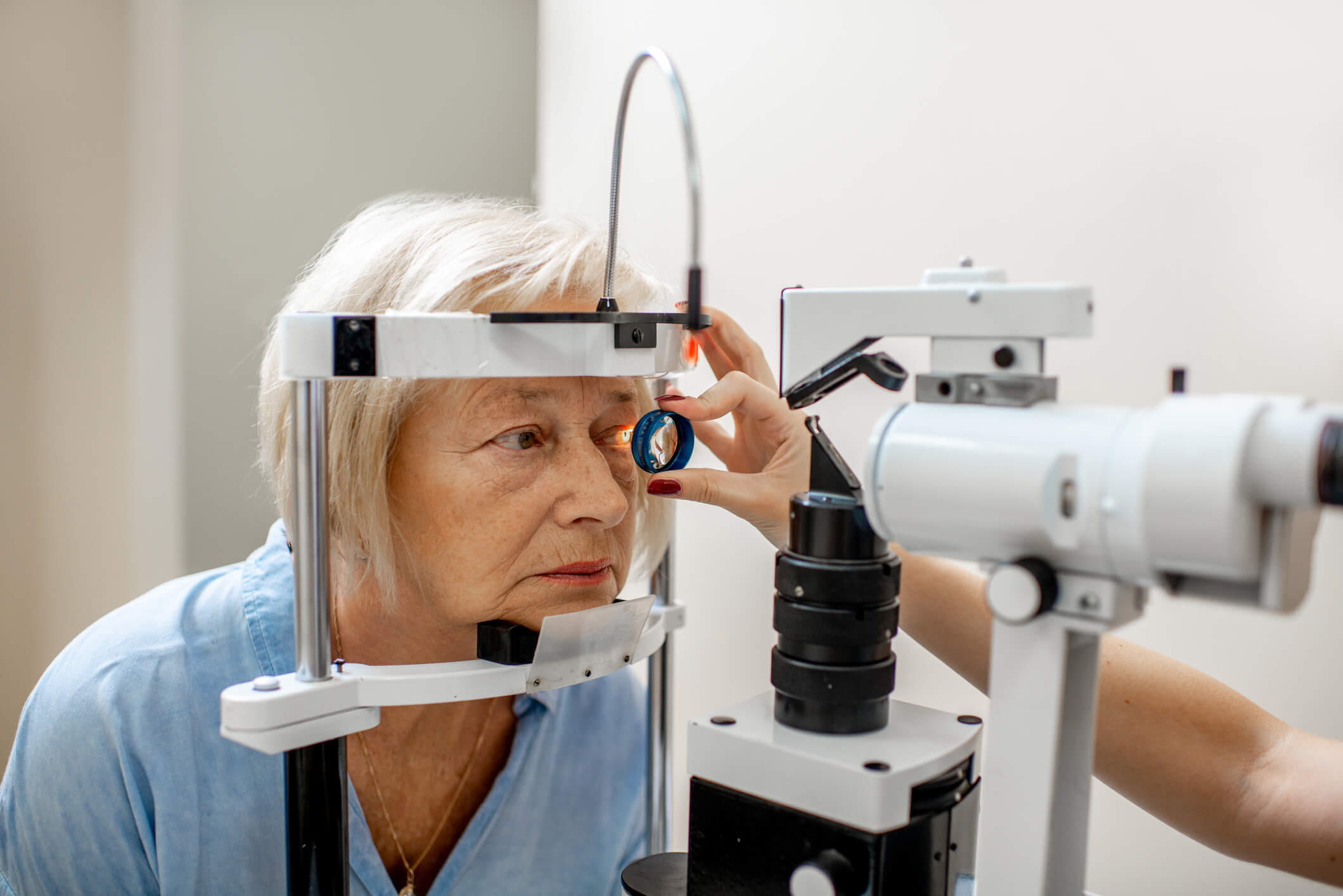
Regular Eye Exams
Equally important is prioritizing regular eye exams. Early detection of changes in IOP or optic nerve health can help manage glaucoma and prevent further vision loss.
By combining a healthy diet, an active lifestyle, and regular check-ups at the eye doctor, you can take steps to protect your vision and overall well-being.
Reliable and Comprehensive Glaucoma Care at Visionary Eye Doctors
At Visionary Eye Doctors, we tailor our eye care services to your specific needs and goals. Whether you’re managing the early stages of glaucoma or just need a routine eye exam, our team is here to create a personalized treatment plan that works for you. With offices located in the Washington, DC and Maryland areas, we make it easy for you to access expert care.
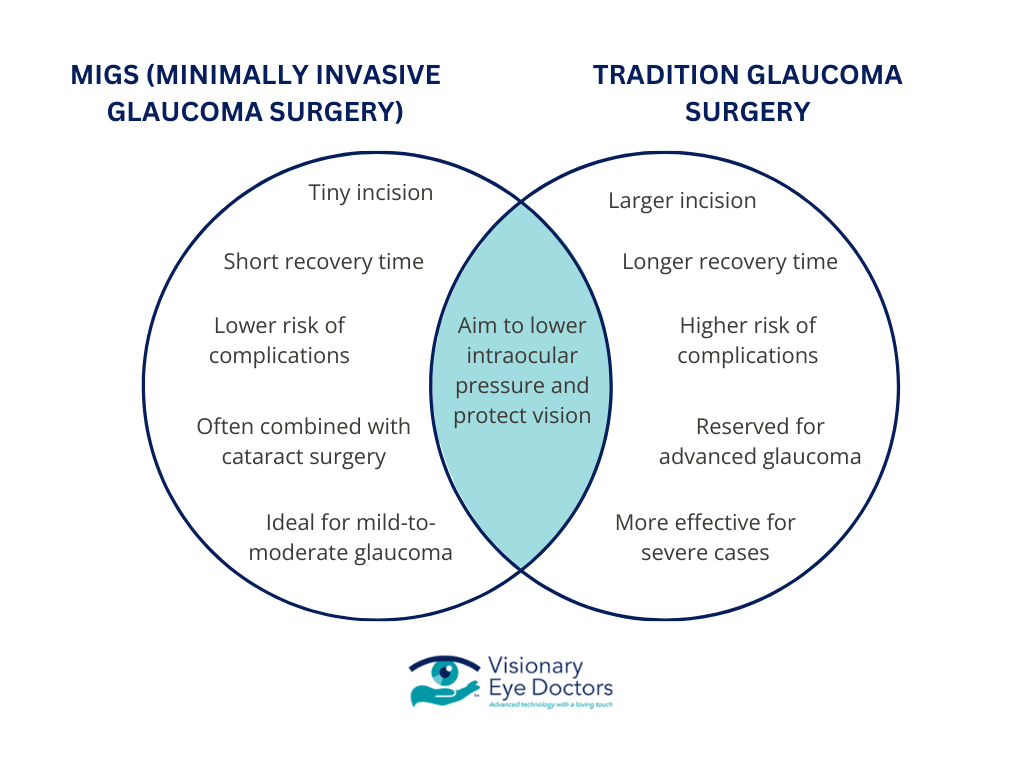
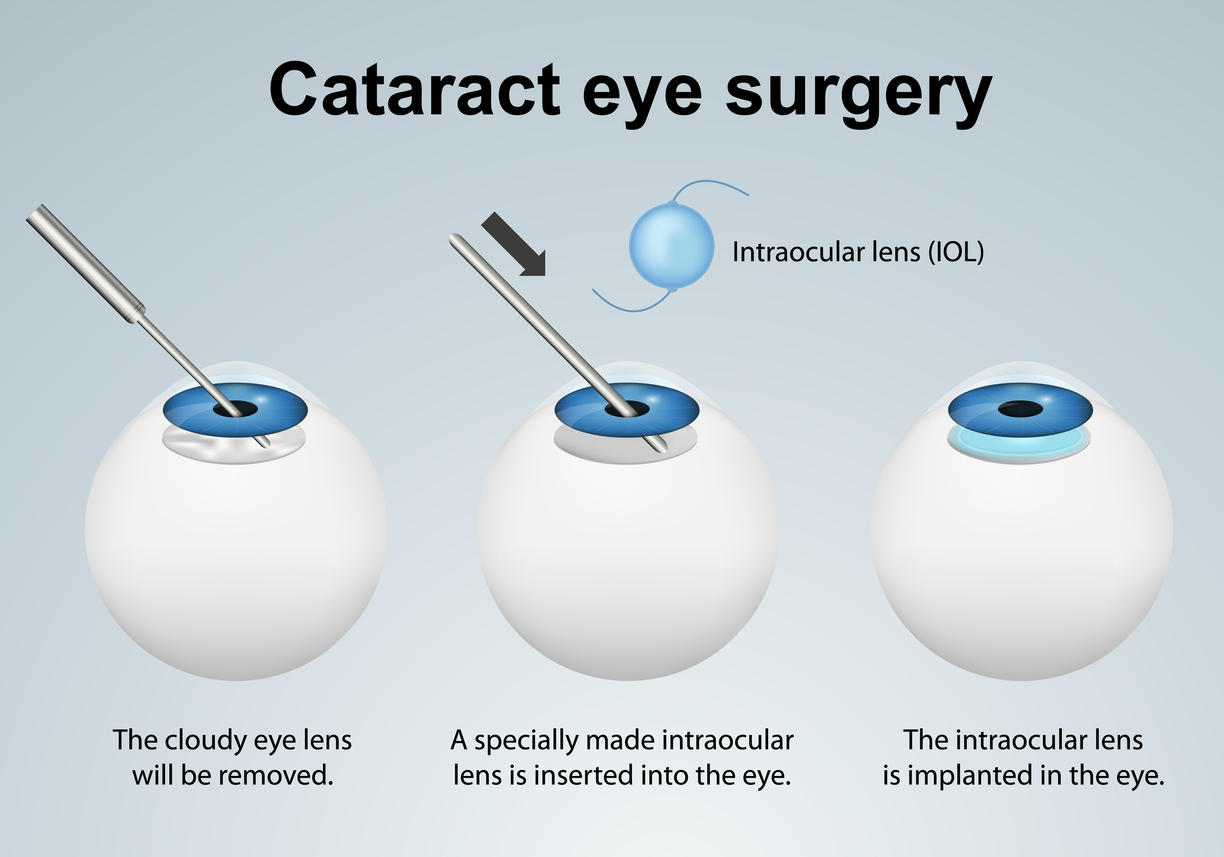
Expertise in Advanced Glaucoma Treatment
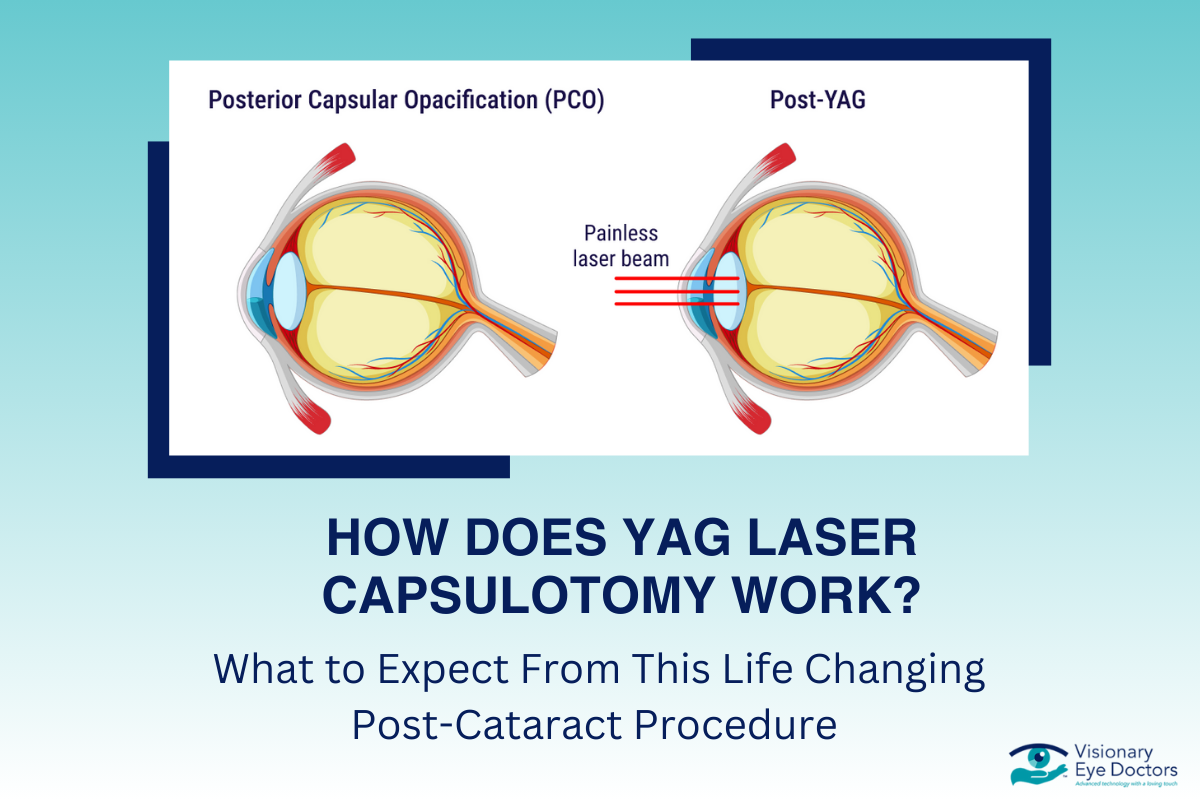
Our eye doctors specialize in all forms of glaucoma, from early diagnosis to advanced treatment options. We also offer expertise in cataract surgery, dry eye, contact lenses, and other eye care services to ensure your eyes remain as healthy as possible. Comprehensive eye exams are at the core of what we do, and these help us detect issues early on so we can protect your vision for the long term.
Take the Next Step. Request an Appointment.
Your eye health is too important to leave to chance. Schedule an appointment with Visionary Eye Doctors today and let our team help you maintain clear, healthy vision.
Resources: